Healthcare Interoperability Solutions for Connected Care
Think of healthcare interoperability solutions as a universal translator for medicine. They create a common language that allows completely different systems, from hospitals and labs to specialist clinics, to share critical patient information securely. This isn’t just a technical upgrade; it’s a foundational shift needed to build a safer and more efficient healthcare system.
Why Connected Care Is No Longer Optional
Imagine trying to solve a complex puzzle with most of the pieces missing. That’s what doctors face every day. Crucial patient data like allergies, medical histories, lab results, and imaging scans are often stuck in isolated digital systems, unable to flow between the very providers who need them most.
This fragmentation creates dangerous information gaps. It leads to redundant tests, delayed diagnoses, and, in the worst cases, preventable medical errors. The cost of this disconnect is staggering, both in dollars and in patient well-being.
When a patient shows up in an emergency room, clinicians can waste precious minutes or even hours just trying to track down their records. This inefficiency drives up administrative overhead, contributing to the estimated $1 trillion spent annually on U.S. healthcare administration. More importantly, it forces providers to make critical decisions with an incomplete picture of a patient’s health.

The Consequences of Data Silos
Disconnected systems create a domino effect of problems that impact everyone involved. The root of the issue is simple: valuable information gets locked away, unavailable at the point of care where it could make a real difference.
This leads to several critical breakdowns:
-
Impaired Patient Safety: A doctor might prescribe a medication that a patient is allergic to, simply because that allergy information is trapped in another provider’s electronic health record.
-
Increased Healthcare Costs: Clinicians often order duplicate lab work and imaging scans because they can’t access prior results. This means unnecessary expenses for patients, insurers, and the system as a whole.
-
Poor Patient Experience: Patients are forced to become couriers for their own medical records, physically carrying files from one office to another or endlessly filling out the same tedious forms for every new specialist.
The need for a change is undeniable. True interoperability is the only way forward to a more efficient, sustainable healthcare system that delivers real value and puts patients first.
Moving Toward a Connected Future
The industry’s shift toward value-based care, where providers are paid for positive patient outcomes, not just the number of services they perform, makes interoperability a must-have. To thrive in this model, organizations need a 360-degree view of the patient’s entire health journey.
This is where a skilled AI solutions partner can be a game-changer, helping to put the right frameworks in place to unlock and make sense of health data. By building these digital bridges between isolated systems, interoperability solutions lay the groundwork for a future where healthcare is genuinely coordinated, proactive, and centered around the patient.
Understanding the Four Levels of Interoperability
Getting to true healthcare interoperability isn’t a one-and-done deal. It’s more like a journey with four key milestones, each one building on the last. Think of it like learning how to have a real conversation in another country.
First, you need a way to connect – a phone line. Then, you have to agree on grammar so your sentences make sense. After that, you need to understand the meaning behind the words. And finally, you establish the social and legal rules for a productive, trusting dialogue. This framework helps break down the complex path toward building truly connected healthcare interoperability solutions.
Level 1: Foundational Interoperability
The first step is what we call Foundational Interoperability. This is all about getting the pipes connected. It simply ensures that one system can securely send a packet of data and another system can receive it.
That’s it. There’s no understanding of what’s inside the packet. It’s like a mail courier delivering a sealed envelope; they can confirm it got from point A to point B, but they have no clue what the letter says. This is the bedrock connection that everything else is built on.
Level 2: Structural Interoperability
Once you have a connection, you need to agree on a format. This is Structural Interoperability, and it’s about giving the data a common grammar or syntax. It defines the structure so the information can be read at the individual data field level.
This ensures both the sending and receiving systems are organizing information the same way. Standards like Health Level Seven (HL7) are the rulebook here, dictating how medical data should be formatted. Going back to our analogy, this is like making sure both parties structure their sentences with a subject, verb, and object, even if they don’t yet understand the full meaning of the words.
As we explored in our guide on hospital system integration services, getting this structure right is an absolute cornerstone of effective data sharing.
Level 3: Semantic Interoperability
This is where the magic really happens. Semantic Interoperability means two or more systems can exchange information and actually use it. It’s about shared understanding; ensuring that the data’s context and meaning are preserved across systems.
Frankly, this is the toughest but most critical level to get right. It depends on everyone agreeing to use the same dictionary for medical terms. Without it, a diagnosis for “heart failure” in one EHR might be completely misinterpreted by another, which could lead to devastating clinical errors.
Key enablers for this shared dictionary include:
-
SNOMED CT: A massive clinical vocabulary for diagnoses and procedures.
-
LOINC: The go-to standard for lab tests and clinical observations.
-
RxNorm: A system for normalizing the names of clinical drugs.
Level 4: Organizational Interoperability
The final piece of the puzzle is Organizational Interoperability, and it has less to do with technology and more with people and policies. This level covers the governance, legal agreements, and trust frameworks that let different organizations exchange data securely and with confidence.
It’s the handshake agreement backed by policy. This is where you establish the rules of engagement for things like patient consent, data security, and complying with regulations like HIPAA.
Organizational interoperability makes sure the right information gets to the right people, at the right time, and for the right reasons. It’s only by climbing all four of these levels that a healthcare system can move from just swapping data to delivering truly connected care that improves patient outcomes and makes the whole system run better.
A Practical Breakdown of Interoperability Levels
To bring these concepts to life, it helps to see them side-by-side. The table below breaks down each level with a simple analogy to make the differences crystal clear.
| Level of Interoperability | Core Function | Example Technologies/Standards | Real-World Analogy |
|---|---|---|---|
| Foundational | Establishes a basic connection for data to move from one system to another. | TCP/IP, Ethernet, WiFi | The mail carrier delivering a sealed envelope. They confirm delivery but don't know what's inside. |
| Structural | Defines a common format or syntax so data can be organized and interpreted at the field level. | HL7 v2, FHIR, XML | Both parties agreeing to write in complete sentences (subject, verb, object) so the structure is readable. |
| Semantic | Ensures shared meaning and context, so the exchanged data is correctly understood and usable. | SNOMED CT, LOINC, RxNorm | Both parties using the same dictionary (e.g., Oxford English Dictionary), so words have the same meaning. |
| Organizational | Provides the governance, policies, and trust frameworks for seamless cross-entity data sharing. | Data Use Agreements (DUAs), HIPAA, GDPR | The formal treaty or business contract that governs how two countries or companies will interact and share resources. |
Each level is a crucial step in the journey. Without the foundational pipes, there's no connection. Without structure and semantics, there's no understanding. And without organizational alignment, there's no trust.
Navigating Key Standards Like FHIR and HL7
To make any sense of health data exchange, you first need to understand the rulebook. In healthcare, that rulebook is a set of critical standards that dictate how information is structured and shared. Without them, it's chaos, like trying to have a conversation where everyone is speaking a completely different language.
At the center of the modern conversation is FHIR (Fast Healthcare Interoperability Resources). Pronounced "fire," this standard has quickly become the go-to for developers and health IT pros, and for good reason. FHIR was built to solve the headaches that came with older, more rigid standards.
It uses a modern, API-first approach that’s built on familiar web technologies like RESTful APIs and JSON. This makes it far more flexible and intuitive for developers, which means new web and mobile health apps can be built much faster.
The Evolution from HL7v2 to FHIR
To really grasp why FHIR is such a big deal, you have to look at what it replaced. For decades, Health Level Seven Version 2 (HL7v2) was the industry workhorse. It was revolutionary in its day, but now it's a legacy standard with some serious limitations. Think of it as a complex, rigid file format that demands specialized knowledge and custom-built parsers for every single integration.
Moving from that rigid structure to a flexible, API-driven model is a game-changer. It’s a fundamental shift in how we think about building connected health systems.
The pyramid below breaks down the different layers needed to get to this kind of meaningful data exchange.
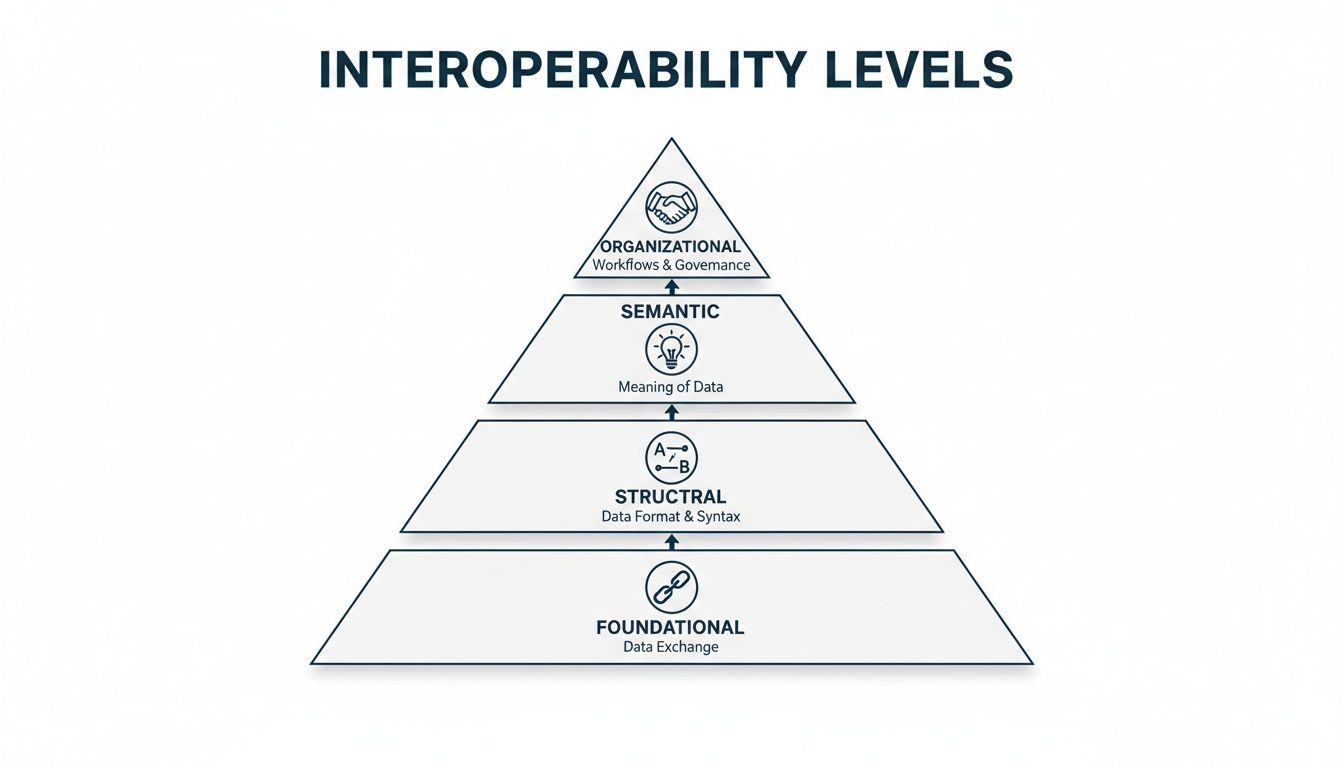
As you can see, standards like FHIR and HL7 are the glue for the structural and semantic levels. They provide the grammar and vocabulary needed to make sure the data isn't just received, but actually understood.
Beyond FHIR: Other Essential Standards
While FHIR gets a lot of the spotlight, it isn't the only player on the field. Different kinds of health information require their own specialized formats.
-
DICOM (Digital Imaging and Communications in Medicine): This is the universal language for medical imaging. Every time a provider pulls up an MRI, CT scan, or X-ray, DICOM is the standard working behind the scenes to ensure the image and its related data are stored and sent correctly.
-
TEFCA (Trusted Exchange Framework and Common Agreement): This isn't a technical standard in the same way. It's a national policy framework in the U.S. designed to create a "network of networks." TEFCA lays down the rules of the road for secure health information exchange on a nationwide scale.
The push for these frameworks is lighting a fire under the market. The global healthcare interoperability solutions market is exploding, valued at $3.94 billion and projected to hit $5.61 billion. This growth is being supercharged by initiatives like TEFCA, which now connects multiple Qualified Health Information Networks (QHINs), allowing over 625 hospitals to exchange data across the country without needing custom agreements – slashing transaction costs in the process. North America currently holds a dominant 42.23% market share, driven by federal mandates from the ONC and hefty information-blocking penalties that can reach $1 million per violation under the 21st Century Cures Act. This has made adopting HL7 FHIR R4 a board-level priority for many organizations.
Choosing the right standards is a make-or-break decision for any health-tech project. Beyond the tech stack, a deep understanding of HIPAA compliance for healthcare providers is non-negotiable for building connected care. As we've covered in our deep dive on software engineering in healthcare, these technical and regulatory pieces have to fit together perfectly. The goal isn't just to build compliant systems, but to build smart, future-proof solutions that genuinely improve patient outcomes. Mastering this language of standards is the first step.
Building Your Implementation Roadmap
Putting healthcare interoperability solutions in place is about much more than just picking the right technology. It’s a journey that demands a clear, strategic roadmap. To get from abstract ideas to a working system, you need a phased approach that accounts for every technical detail and organizational hurdle along the way.
A solid roadmap is your best defense against costly mistakes. It breaks down what feels like a massive project into smaller, manageable stages, giving everyone from your dev team to your executive sponsors a clear sense of direction.
Phase 1: Discovery and Strategy
Before you write a single line of code, you have to define what success actually looks like. This first phase is all about deep analysis and getting everyone aligned. You need a complete picture of your current tech stack, a clear-eyed view of the data silos you’re trying to break down, and a firm grasp on the business goals driving the entire project.
Key activities here include:
-
Stakeholder Interviews: Talk to everyone. Sit down with clinicians, administrators, IT staff, and even patients to understand their biggest data-sharing headaches and what they need to make their lives easier.
-
System Audits: Map out every system you have, from that old legacy EHR that won't die to your modern billing platform. This helps you identify all your data sources and anticipate integration challenges.
-
Defining KPIs: Get specific about how you'll measure success. Is it a reduction in redundant lab tests? Faster patient intake times? Better care coordination scores? Pin it down now.
This strategic foundation is everything. Without it, you could build a technically perfect solution that solves all the wrong problems.
Phase 2: Architecture Design and Data Mapping
Once you have a clear strategy, it's time to draw up the technical blueprint. This is where you decide on the core architecture and integration patterns that will serve as the backbone for your entire interoperability framework. It’s all about making smart decisions on how data will flow between systems – securely and efficiently.
Two common patterns you’ll run into are:
-
API Gateway: This is a great fit for modern, service-oriented architectures. An API gateway acts as a single, managed front door for all data requests. It simplifies security, monitoring, and traffic management, especially when you're connecting to mobile or web apps using FHIR.
-
Central Integration Engine: If you're wrestling with a bunch of legacy systems that all speak different languages (like HL7v2), a central integration engine is often a must. Think of it as a universal translator, converting and routing data between systems that can't talk to each other directly.
With the architecture decided, the really meticulous work of data mapping begins. This process is all about defining exactly how a piece of information in one system corresponds to data in another. For example, mapping a "patient ID" from an old EHR to the "medical record number" in a new system is absolutely critical for keeping your data clean and accurate.
A common pitfall is underestimating the complexity of data mapping. It's not just a technical task but a clinical one, requiring input from those who understand the context and meaning of the data.
Phase 3: Security, Governance, and Testing
With the blueprint ready, the final phase is all about building a system that’s secure, compliant, and rock-solid. This means setting up strict data governance rules, implementing ironclad security, and designing a bulletproof testing strategy. As we explored in our guide on healthcare software modernization, getting these foundational elements right is what separates successful projects from failed ones.
Data governance sets the rules of the road: who can access what data, under what circumstances, and for what reason. It's how you ensure compliance with regulations like HIPAA and build trust across the board.
Security protocols are non-negotiable. This includes:
-
End-to-End Encryption: Protecting data whether it’s sitting on a server or moving between systems.
-
Robust Authentication: Using multi-factor authentication and role-based access controls to ensure only authorized users get in.
-
Continuous Monitoring: Actively watching for and responding to potential security threats in real-time.
Finally, a multi-layered testing strategy is essential to prove the whole thing works as intended. This goes way beyond simple unit tests. We're talking end-to-end integration testing, performance testing under heavy loads, and user acceptance testing with your clinical staff to make sure the new workflows are actually practical and intuitive. By following this phased roadmap, you can navigate the complexities of implementation and build an interoperability solution that delivers real, lasting value.
How AI Supercharges Your Interoperability Strategy
Think of interoperability as building a superhighway for health data. It's the critical infrastructure that gets information moving freely and securely between different systems. But just having the highway isn't the endgame. The real magic happens when you start intelligently managing the traffic. This is where Artificial Intelligence (AI) comes in, turning your data pipeline into a learning, thinking system.
Interoperability gets the data flowing; AI makes it smart. Once information from EHRs, labs, and imaging systems is finally in a common, accessible format, AI and machine learning algorithms can analyze it at a scale and speed no human ever could. This is how a static repository of patient information becomes a living asset, one that actively sharpens clinical decisions and smooths out operations. It’s the step that delivers a real return on your data integration investment.

From Connected Data to Predictive Insights
One of the most powerful things you can do with AI in an interoperable environment is predictive analytics. With a complete view of a patient's history, AI models can spot the subtle patterns that scream "high risk" for things like hospital readmissions, sepsis, or the progression of a chronic disease.
This shifts the entire care model from reactive to proactive. Imagine an AI system flagging a diabetic patient who, based on recent lab results, pharmacy records, and data from their glucose monitor, is on a dangerous path toward kidney failure. The care team gets an alert and can intervene now, adjusting the treatment plan long before the condition escalates. This is a game-changer for improving patient outcomes and bending the cost curve.
The global momentum for this synergy is undeniable. A recent Black Book survey of over 21,000 users found that interoperability was the non-negotiable "price of entry" for any new platform. A staggering 92% of fast-adopting markets listed FHIR/API capabilities as a top-three requirement. Those forward-thinking nations are already seeing the payoff, with 12 points higher deployment of production-grade clinical AI.
Unlocking the Value in Unstructured Data
A huge chunk of clinical data, some estimates say up to 80%, is unstructured. We're talking about doctors' notes, discharge summaries, and pathology reports. This information is loaded with vital context, but it's basically invisible to traditional analytical tools.
This is where Natural Language Processing (NLP), a specialized field of AI, becomes absolutely essential. NLP algorithms can be trained to "read" and understand human language. They can pull out key facts from messy, unstructured text and turn them into standardized data that a system can actually use.
By applying NLP, a health system can automatically scan thousands of clinical notes to find patients who are perfect candidates for a new clinical trial. Or it could monitor for adverse drug events in real-time across the entire patient population. It’s about turning messy, text-based notes into a structured asset for research and patient safety.
For example, high-quality dictation software for medical professionals powered by AI not only speeds up documentation but also helps create the structured data needed for these interoperable systems to work in the first place.
Automating Workflows and Reducing Burden
AI isn't just for high-level clinical insights. It's also an incredibly effective tool for tackling the soul-crushing administrative work that leads to provider burnout. Intelligent automation can handle the repetitive, rules-based tasks, giving your clinical staff more time to focus on what they do best: care for patients.
Here are a few practical examples:
-
Automated Prior Authorization: Instead of staff spending hours on the phone, an AI can analyze patient data against payer rules to automatically assemble and submit prior authorization requests. This means less waiting and faster care.
-
Intelligent Claims Processing: Machine learning models can scan medical claims for common errors or potential fraud before they're submitted, drastically cutting down on denial rates and speeding up reimbursement.
-
Smart Scheduling: AI can optimize appointment calendars based on patient needs, provider availability, and equipment use, making the entire operation run more smoothly.
By weaving AI into your interoperability strategy, you finally capitalize on the true promise of all that connected data. You create a powerful feedback loop: connected data feeds intelligent algorithms, which produce insights that lead to better, more efficient care. It’s the definitive way to turn your data from a simple record into a decisive advantage.
Measuring Real-World Impact and ROI
Getting a healthcare interoperability project off the ground means making a serious investment. To get that approved, you have to talk about more than just the tech. It’s all about demonstrating the tangible, real-world results that come from connecting your systems. Success isn't just about data flowing freely; it's about proving the clinical and financial return that follows.
You need hard evidence. How, exactly, does connected data improve patient care? And where does it strengthen the bottom line? The value really breaks down into those two key areas: the immediate, powerful gains on the clinical side, and the cost-saving efficiencies you unlock on the financial side.
Quantifying the Clinical Gains
Let’s be clear: the most important impact of interoperability is on patient care. When a clinician can pull up a complete, real-time view of a patient's history, the quality and safety of the care they provide go up dramatically. This isn’t just a nice idea; it shows up in real, measurable outcomes.
Here are the key clinical metrics you should be tracking:
-
Fewer Medical Errors: Having instant access to comprehensive allergy lists, medication histories, and past diagnoses is a game-changer. It helps prevent adverse drug events and other mistakes that, unfortunately, are a leading cause of harm in healthcare.
-
Tighter Care Coordination: Think about the journey of a patient with a chronic condition. When their primary care doctor, specialists, and the local hospital can all see the same chart, care transitions become much smoother and safer.
-
Happier Patients: Patients notice the difference immediately. They no longer have to repeat their entire medical history at every single appointment or act as a courier for their own records. That seamless experience builds trust and keeps them coming back.
Tracking the Financial ROI
While better patient outcomes are the ultimate goal, you won't get executive buy-in without a rock-solid financial case. The worldwide healthcare interoperability market is expected to jump from $7.34 billion to a staggering $16.49 billion by 2034. That growth is fueled by the 84% of global healthcare organizations that now see interoperability as fundamental to better care.
Organizations that are moving fast are already seeing undeniable ROI. They're making use of 43% more of their EHR data outside of their own four walls, powering new patient-centered platforms and services. Explore the latest trends in EHR and interoperability to see where the industry is headed.
The financial argument for interoperability is built on one word: efficiency. When you eliminate information gaps and automate data exchange, you slash wasted resources and administrative friction.
Looking at some of our own client cases, we've seen firsthand how a shared data platform can drive a 15% reduction in hospital readmission rates – a metric that comes with significant financial penalties.
But the wins don't stop there. You also see savings from eliminating redundant lab tests, cutting administrative costs tied to manual data entry, and qualifying for value-based care incentives that directly reward better outcomes. When you connect these operational improvements to clear financial metrics, you can prove that interoperability isn't just a cost center. It’s a strategic investment in a more efficient, sustainable future.
Frequently Asked Questions About Interoperability
It’s natural to have questions when you’re digging into the world of healthcare interoperability solutions. It's a complex topic, so let's clear up a few of the most common ones we hear from leaders in the field.
What Is the Biggest Challenge in Achieving Interoperability?
You might think the hardest part is the technology, like wrestling with old legacy systems. While that's certainly a headache, the real roadblocks are usually organizational.
The biggest hurdles we see are inconsistent data standards from one institution to the next, a lack of clear governance, and a deep-seated cultural resistance to sharing information. These hesitations often stem from competitive fears or privacy concerns. As we covered in the implementation roadmap, getting this right requires strong leadership and collaborative policies just as much as it requires the right technology from a trusted AI solutions partner.
How Is FHIR Different From Older Standards Like HL7v2?
FHIR is a huge leap forward. The older standards, like HL7v2, were often rigid, complex, and difficult to work with. FHIR, on the other hand, was built using modern web standards like RESTful APIs and uses formats like JSON that developers are already comfortable with.
Think of it this way: HL7v2 is like a clunky, proprietary file format from the 90s. FHIR is like a flexible, universal web API that's easy to plug into any modern web or mobile app created through custom software development. It’s simply faster and more intuitive to build with.
Are Interoperability Solutions Only for Large Hospitals?
Absolutely not. That might have been true in the past, but the game has changed. Today, the rise of cloud platforms and API-first services has put powerful interoperability tools within reach for organizations of all sizes.
Smaller clinics, specialty practices, and even startups can now tap into managed services to connect with major Health Information Exchanges (HIEs) and national networks. They get all the benefits without having to build a mountain of infrastructure themselves.
This shift has really lowered the barrier to entry, allowing more innovators to contribute to a connected care system. With the right healthcare software development partner, these solutions can be scaled to fit any need. It’s the first step toward unlocking the real power of AI for your business.
Ready to build a truly connected healthcare ecosystem? The expert teams at Bridge Global specialize in creating intelligent, compliant, and scalable healthcare interoperability solutions. We combine deep industry knowledge with cutting-edge AI development services to break down data silos and unlock the true potential of your health information. Explore our client cases and discover how we can help you deliver better patient outcomes and drive operational efficiency.



