Harness EHR Integration Services to Unify Patient Data
At their core, EHR integration services are specialized IT services that connect your primary Electronic Health Record (EHR) system with all the other software you use. It’s about building digital bridges between what are often isolated islands of data.
Think of it this way: your lab system, your billing software, your patient portal, and your main EHR are all holding crucial pieces of a patient’s story. Integration services bring those pieces together, creating a single, complete view of their medical history. This connectivity is the key to cutting down on clinical errors, improving how your care teams work together, and making the whole operation run more smoothly.
Why EHR Integration Is No Longer Optional in Modern Healthcare
If you’ve ever worked in a hospital or clinic, you’ve seen the data silos. The billing department’s system can’t talk to the lab’s, and neither can easily push information into the main EHR. This fragmentation creates a choppy, broken experience for both patients and clinicians.
Doctors and nurses end up chasing down information, sometimes ordering duplicate tests or making critical decisions with an incomplete picture of the patient’s health. The results are frustrating at best: administrative headaches and wasted money, and dangerous at worst, posing serious risks to patient safety.
This is where EHR integration services step in, acting as a universal translator. They get all your different software, from the pharmacy management system and radiology imaging platforms to telehealth tools, speaking the same language. By breaking down these data barriers, integration builds that single, coherent patient story that your providers can access whenever and wherever they need it.
The Strategic Value of a Connected Health Ecosystem
It’s easy to see integration as just another IT project, a technical box to check. But that view misses the forest for the trees. This is a strategic investment in creating a more resilient, efficient, and patient-focused healthcare organization.
The market reflects this shift. The demand for these services is exploding, with the wider U.S. Electronic Health Records market projected to reach US$50.78 billion by 2033. This growth isn’t just about technology; it’s about providers recognizing that seamless data exchange is the engine that powers all other modern digital health initiatives. You can find more details on the market’s growth in recent industry reports.
When done right, a solid integration strategy delivers tangible benefits that ripple across the entire organization:
-
Smarter Clinical Decisions: Clinicians get a complete, real-time view of a patient’s history, allergies, medications, and lab results. This leads directly to more accurate diagnoses and safer treatment plans.
-
Smoother Operations: By automating workflows and eliminating manual data entry, you reduce redundant tasks. This frees up your staff to focus on what they do best: taking care of patients.
-
Better Patient Outcomes: Coordinated care isn’t just a buzzword. When specialists and departments are on the same page, patient transitions and follow-ups are smoother, which is absolutely critical for managing chronic conditions.
-
A Healthier Bottom Line: Integration drives more accurate billing and faster claims processing. When your clinical and financial data are in sync, you see fewer claim denials and a stronger revenue cycle.
By unifying all these different data sources, EHR integration turns fragmented information into genuinely useful clinical intelligence. It’s the foundation for almost every major innovation in healthcare today, from population health analytics to personalized medicine.
Getting through the complexities of integration requires a partner who brings both great technical skill and real-world healthcare experience to the table. As an experienced AI solutions partner, Bridge Global helps healthcare organizations forge these vital connections, turning siloed data into a powerful asset for delivering better care. As we’ve covered before, having the right healthcare IT solutions is the first step toward achieving true interoperability.
Understanding the Technologies That Power EHR Integration
To get different healthcare systems talking to each other, you need a powerful combination of technologies working together. Think of it less like a single solution and more like a carefully assembled toolkit, where each tool has a specific job. Getting EHR integration services right means knowing which tools to use and how to make them work in concert.
At the core of it all is the need for a common language. For decades, the industry’s default language was HL7 (Health Level Seven).
The Foundation: HL7 and FHIR
HL7 V2 was the workhorse standard that brought order to the chaos. It’s a very strict, detailed set of rules for formatting and sending essential healthcare information, such as patient admissions, lab results, or billing data. It’s incredibly thorough but also very rigid. Every system had to follow its pipe-and-hat delimited format precisely, making it a reliable but often inflexible solution for legacy systems.

But as healthcare embraced the web and mobile apps, the old way of doing things just couldn’t keep up. That’s where FHIR (Fast Healthcare Interoperability Resources) came in.
If HL7 is like a dense, technical instruction manual, FHIR is more like a set of universal LEGO blocks. It’s built on modern web standards that developers already know, which makes building new connections much faster and less painful.
FHIR breaks down massive health records into small, logical chunks called “Resources” – like a ‘Patient’ resource, a ‘Medication’ resource, or an ‘Appointment’ resource. This modular approach is key to building the kind of agile systems we discuss in our guide on engineering digital health platforms.
The Connective Tissue: APIs and Middleware
Having a standard language like HL7 or FHIR is great, but you still need a way to actually send and receive the messages. That’s the job of APIs and middleware.
-
APIs (Application Programming Interfaces): Think of an API as a secure messenger. It’s a set of rules that lets one application ask another for a specific piece of information and get a response. For example, a patient portal app can use an API to ask the EHR for upcoming appointments. It gets just the data it needs, without ever exposing the entire, complex EHR database.
-
Middleware: When you have dozens of different systems trying to talk to each other, connecting them one by one creates an unmanageable mess. Middleware acts as the central traffic cop. It sits in the middle of everything, directing the flow of data, translating between different formats (like converting an old HL7 message into a modern FHIR resource), and making sure every message gets to its destination.
Middleware is the secret to scalable integration. It prevents a “spaghetti architecture” of tangled point-to-point connections, creating a clean, manageable, and secure hub for all data exchanges.
A smart integration strategy combines these elements. For example, your middleware platform could take a legacy HL7 message from an old lab system, instantly translate it into the FHIR format, and then use a modern API to push that data to a doctor’s smartphone app.
This combination of standards, messengers, and traffic controllers is what makes a truly connected healthcare ecosystem possible.
Comparing Key EHR Integration Standards and Architectures
To help you understand how these pieces fit together, the table below breaks down the most common technologies used in EHR integration. It outlines what they are, how they work, and where they shine, giving technology leaders a clear snapshot for making strategic decisions.
| Technology | Primary Use Case | Data Structure | Flexibility | Best For |
|---|---|---|---|---|
| HL7 v2 | Legacy system data exchange (admissions, orders, results). | Segment-based, pipe-and-hat delimited text. | Low | Connecting established, on-premise clinical systems like labs and radiology. |
| FHIR | Modern web and mobile app integration. | Resource-based (JSON/XML). | High | Powering patient portals, telehealth apps, and third-party integrations. |
| APIs | Secure, real-time data requests between applications. | Varies (often RESTful with JSON). | High | Enabling specific, controlled access to data for any application. |
| Middleware | Centralized data routing and transformation. | Manages multiple formats. | High | Orchestrating data flow in complex environments with many disparate systems. |
Ultimately, choosing the right mix of these technologies isn’t a one-size-fits-all decision. It really depends on your organization’s unique goals, the systems you already have in place, and where you plan to go in the future.
Navigating Security and Compliance in Healthcare Data
In healthcare, data isn’t just data. It’s a patient’s story, a critical diagnosis, a life-altering treatment plan. That’s why protecting this information isn’t just a good IT practice; it’s a legal and ethical duty. When you engage in EHR integration services, you’re building new digital pathways for this sensitive information to travel. Making sure those pathways are secure from day one is absolutely non-negotiable.
This is where regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. and the General Data Protection Regulation (GDPR) in Europe come in. They aren’t just rulebooks; they are the bedrock of patient trust. These frameworks set strict standards for how Protected Health Information (PHI) is handled, stored, and shared, ensuring every piece of data gets the respect and protection it deserves.
The Pillars of a Secure Integration Strategy
A truly secure integration isn’t about a single magic bullet. It’s about building multiple layers of defense that work together. Think of it like a medieval castle; you need high walls, alert guards, and a detailed log of everyone who comes and goes. Each security layer closes a different potential loophole.
Here are the essential security protocols that must be part of your integration architecture:
-
End-to-End Encryption: This is your first and most important line of defense. It scrambles data from the moment it leaves one system until it safely arrives at its destination. Even if a cybercriminal managed to intercept it, they’d just get a useless jumble of characters.
-
Robust Access Controls: Not everyone needs to see everything. Role-Based Access Control (RBAC) is a smart way to ensure that clinicians, billing staff, and administrators can only access the specific information they need to do their jobs. This “least privilege” principle is a powerful tool against internal breaches.
-
Multi-Factor Authentication (MFA): Passwords alone just don’t cut it anymore. MFA adds a vital second step, like a code sent to a phone, to verify a user’s identity before they can access sensitive systems.
-
Comprehensive Audit Trails: A secure system has to keep a meticulous record of every action. Detailed logs track who accessed what data, when they did it, and what changes they made. These trails are essential for spotting suspicious activity and are a core requirement for HIPAA compliance.
A robust integration strategy is inherently a secure one. Compliance isn’t an afterthought or a final checkbox; it’s a guiding principle that shapes every decision in the architecture, development, and deployment process.
Beyond the Basics: Proactive Security Measures
Real security means being proactive, not just reactive. It’s about constantly looking for weaknesses before attackers do. This involves conducting regular vulnerability assessments and penetration testing to find and fix security gaps.
It also means holding your partners to the same high standards. Any third-party system you connect with, from a diagnostic lab to a patient portal, must share your commitment to data protection. Understanding how to maintain patient confidentiality in healthcare AI is especially critical as these tools become more integrated.
For a closer look at the technical details, as we explored in our guide on HIPAA-compliant application development, achieving compliance goes much deeper. For any CIO or compliance officer, the mission is simple: create a connected healthcare ecosystem where data flows seamlessly to those who need it, but remains an impenetrable fortress to everyone else.
Your Step-by-Step EHR Integration Project Roadmap
Kicking off an EHR integration project can feel a lot like preparing for a major expedition. You need a clear map, the right crew, and a very specific destination in mind. This roadmap is designed to cut through the complexity, breaking the journey into manageable phases that will guide you from a simple idea to a successful, long-term solution.
A well-structured plan is what turns a daunting technical project into an achievable business goal. It gets everyone on the same page, from the executive suite to the front-line clinical staff, ensuring you’re all working towards a shared vision of seamless data flow.
Phase 1: Discovery and Strategic Planning
This is where you lay the groundwork and figure out what a “win” actually looks like. Before anyone even thinks about writing code, your team needs to get together and answer some tough questions about the project’s real purpose and scope. This phase isn’t just about the tech; it’s about making sure the integration solves real clinical and business problems.
Here’s what you’ll tackle first:
-
Define Your Goals: Get specific about what you need to achieve. Are you trying to slash administrative busywork, give doctors better insights for decision-making, or speed up your revenue cycle?
-
Align Stakeholders: Pull your clinical, administrative, and IT teams into the same room. This is the only way to guarantee the final product solves real-world workflow headaches, not just technical puzzles.
-
Audit Your Systems: Take a deep dive into your current tech stack. You need to document every system’s capabilities, data formats, and any API limitations that could throw a wrench in the works.
One of the biggest mistakes we see is teams jumping straight into development. Taking the time to plan meticulously upfront saves an incredible amount of time, money, and frustration down the road.
Phase 2: Architecture Design and Vendor Selection
Once your goals are crystal clear, it’s time to draw up the technical blueprint. This is where you decide on your integration architecture. Will you go with a centralized middleware approach, simple point-to-point connections, or maybe a hybrid model? The right choice hinges on your organization’s size, budget, and where you see yourself in the next five years.
This is also when you’ll pick your technology partner. You need a team with proven experience in EHR integration services, a rock-solid grasp of standards like HL7 and FHIR, and a portfolio of successful projects you can look at. A partner who specializes in healthcare software development brings a level of industry know-how that’s simply invaluable.
Phase 3: Development and Rigorous Testing
Now, the architectural plans start turning into a real, functional system. The development team gets to work building the connectors, APIs, and data transformation logic that will let your systems talk to each other. For organizations with very specific workflows, this often requires some custom software development to bridge the gaps between standard, off-the-shelf products.
But the most critical part of this phase? Testing. And it’s so much more than just checking if things turn on and off.
-
Unit Testing: Making sure each individual piece of the puzzle works perfectly on its own.
-
Integration Testing: Confirming that all the connected systems can actually pass data back and forth correctly.
-
User Acceptance Testing (UAT): This is where your end-users, the clinicians and admin staff, get their hands on the system. They run it through real-world scenarios to make sure it truly meets their day-to-day needs.
This diagram illustrates how data security is woven into the development process, using encryption, access controls, and auditing to safeguard patient information every step of the way.
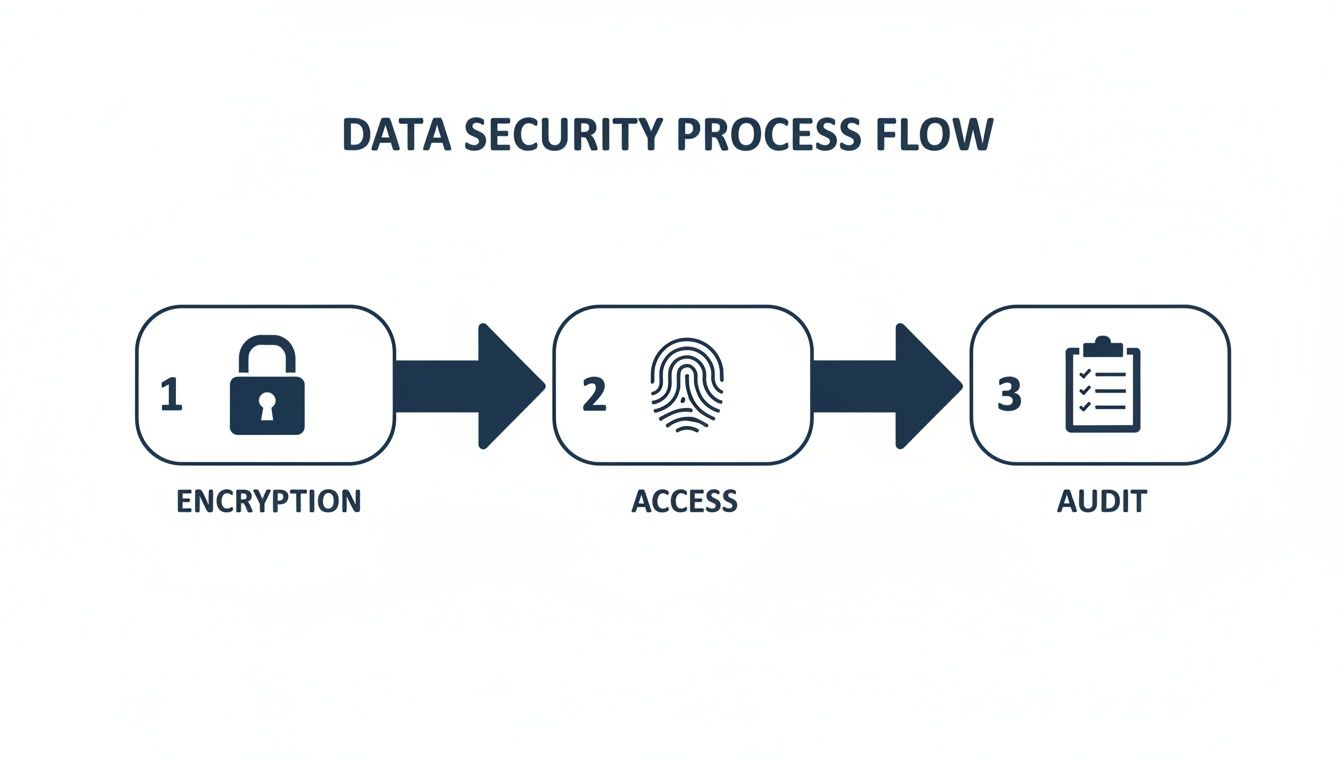
By baking these security protocols directly into the integration workflow, you can be confident that sensitive data stays protected whether it’s moving between systems or sitting in a database.
Phase 4: Deployment and Ongoing Maintenance
After the system has passed every test with flying colors, it’s ready for go-live. A phased rollout is almost always the smartest move. By introducing the new integration to one department or clinic at a time, you minimize disruptions and give your IT team a chance to handle any unexpected issues on a much smaller scale.
But the journey isn’t over once you flip the switch. Ongoing maintenance is what keeps the system running smoothly for the long haul. This means monitoring performance, applying security updates, and tweaking the integration as your organization’s needs change over time. As an AI solutions partner, we also see this as the perfect time to explore how intelligent automation and predictive analytics can make your workflows even smarter.
These evolving workflows are part of a massive industry shift. Milestones like the broad adoption of FHIR, the explosion of telehealth, and the rise of AI in clinical support have completely reshaped modern healthcare. It’s this constant innovation that is fueling a global Medical EHR System market projected to soar to $65 billion by 2033. This huge number reflects the industry’s commitment to building connected, intelligent health platforms. Discover more market trends and forecasts to get the full picture of this growth.
Frequently Asked Questions About EHR Integration Services
Here we answer some of the most common questions healthcare leaders have about planning and executing an EHR integration project.
What are EHR integration services?
EHR integration services are specialized IT solutions that connect an Electronic Health Record (EHR) system with other software applications used in a healthcare organization. This creates a unified data ecosystem, allowing seamless data flow between systems like billing software, lab information systems, patient portals, and telehealth platforms, ultimately providing a single, comprehensive view of patient information.
What is the typical timeline for an EHR integration project?
It varies significantly based on complexity. A simple point-to-point integration using modern APIs could be completed in 4-6 weeks. However, a complex, multi-system project involving legacy platforms and custom development can take 6 to 12 months or longer. A thorough discovery phase is crucial for setting a realistic timeline.
How do you ensure data quality during integration?
Data quality is a continuous process. It starts with data cleansing and validation before migration. During integration, data transformation rules are applied to standardize formats. Post-integration, automated quality checks run continuously to identify and flag any inconsistencies, ensuring the reliability of the unified data.
Who needs to be involved in an EHR integration project?
A successful project requires a cross-functional team. Key stakeholders include executive sponsors, a dedicated project manager, IT specialists (developers, security experts), clinical leaders (physicians, nurses), and administrative staff from departments like billing and scheduling. Involving end-users from the very beginning is critical for user adoption and overall project success.
Choosing the Right Partner and Measuring Your ROI
Picking the right partner for an EHR integration project is just as crucial as the technology itself. Honestly, the success of the whole thing rides on their shoulders. You need a team that gets the unique, often frustrating, complexities of healthcare, not just a group of coders. The best partner isn’t a vendor; they’re a strategic guide who can help you navigate the technical minefield and deliver real improvements for your clinicians and your business.
When you’re vetting potential partners, the first thing to look for is a solid track record in the healthcare world. They need to live and breathe this stuff, with deep knowledge of standards like FHIR and HL7. Don’t be shy about asking to see their client cases. You want proof they’ve solved interoperability problems like the ones you’re facing. A team with a background in healthcare software development will inherently understand the pressures of clinical workflows and the weight of regulatory compliance.
Key Criteria for Selecting Your Integration Partner
To make sure you end up with a team that can actually deliver, keep these qualifications at the top of your list:
-
Deep Healthcare Expertise: This is non-negotiable. They must understand clinical workflows, data privacy laws like HIPAA, and the day-to-day pressures your providers face.
-
Technical Proficiency: Look for proven experience with HL7, FHIR, APIs, and modern middleware. They need to be just as comfortable with your legacy systems as they are with a cutting-edge cloud setup.
-
A Collaborative Approach: The right partner works with your teams: clinical, IT, and administrative, not just for them. They should be obsessed with clear communication and making sure everyone is on the same page.
-
Future-Focused Vision: The best partners don’t just put out today’s fires. They help you build a scalable system that can grow with you and handle whatever comes next, like integrating AI or new patient-facing tools.
Choosing a partner is a long-term commitment. You aren’t just buying a piece of software; you’re investing in a relationship built on trust, shared goals, and a mutual commitment to improving patient care through technology.
Measuring ROI Beyond the Bottom Line
To get buy-in for an investment in EHR integration services, you have to build a rock-solid business case around its return on investment (ROI). While cost savings are a great start, the real value comes from the operational and clinical improvements that spread throughout your organization. A strong case looks past the simple budget line items and measures the wider impact on efficiency, staff well-being, and patient outcomes.
The healthcare industry is well past the early adoption phase – over 95% of U.S. hospitals are using EHRs. Yet, getting these systems to talk to each other remains a massive headache. You have giants like Epic Systems, which holds data for over 60% of U.S. records, alongside thousands of organizations running on MEDITECH or eClinicalWorks. This fragmented landscape is exactly why expert integration partners are so essential. And with over 50% of clinician burnout linked to clunky, disconnected systems, the need for seamless, user-friendly solutions has never been more urgent. You can discover more insights on these EHR statistics and see just how deep this problem runs.
Key Metrics for a Comprehensive ROI Analysis
To build that compelling business case, focus on tracking these key indicators:
-
Reduced Administrative Workload: Measure the time your team gets back by automating manual data entry, scheduling, and billing. A 15-20% cut in administrative time per clinician is a realistic and powerful goal.
-
Improved Clinical Efficiency: Look at metrics like shorter patient wait times, faster access to lab results, and fewer duplicate tests. These aren’t just numbers; they represent better resource use and the ability to see more patients.
-
Lower Clinician Burnout Rates: This one can feel harder to quantify, but tracking staff satisfaction and retention before and after integration tells a powerful story about its impact on your culture.
-
Enhanced Patient Outcomes: Ultimately, this is what it’s all about. Monitor clinical metrics like readmission rates, medication adherence, and how well chronic conditions are being managed.
In the end, a successful integration, guided by the right AI solutions partner, turns your data from a static archive into an active, strategic asset. By bringing in AI development services, you can start unlocking predictive insights and intelligent automation, truly realizing the potential of AI for your business and setting a new standard of care.
Your EHR Integration Questions, Answered
Jumping into an EHR integration project always brings up a lot of questions. We get it. Below, we’ve tackled some of the most common ones we hear from healthcare leaders to clear up any confusion and help you move forward with confidence.
What’s the Real Difference Between HL7 and FHIR?
This is a big one. Think of it like the difference between sending a formal, structured letter versus a modern, flexible email. Both get the message across, but they’re built for different eras and purposes.
HL7 v2 has been the industry’s workhorse for decades. It’s a powerful but very rigid standard, almost like a strict set of grammatical rules for exchanging clinical data. It’s fantastic for ensuring traditional, on-premise systems can talk to each other, but it can feel clunky and outdated when you’re trying to connect newer applications.
FHIR (Fast Healthcare Interoperability Resources), on the other hand, is the new kid on the block. It’s built on the same modern web technologies (APIs) that power the apps on your phone, which makes it far more flexible and easier for developers to work with. FHIR breaks data down into logical “Resources”, like a ‘Patient’ or an ‘Appointment’, which makes it a breeze to build connections for mobile health apps, patient portals, and other digital health tools.
The smartest integration strategies don’t pick one over the other; they use both. FHIR is perfect for connecting new, agile applications to your ecosystem, while HL7 v2 can continue its reliable work handling communication with your deeply embedded legacy systems.
An experienced partner in healthcare software development can help you design a hybrid architecture that plays to the strengths of both standards, giving you the best of both worlds.
How Long Does an EHR Integration Project Actually Take?
This is the million-dollar question, and the honest answer is: it completely depends on the project’s complexity and scope.
A fairly straightforward integration, say, connecting two modern systems that both have well-documented, FHIR-based APIs, can be surprisingly quick. We’re talking a few weeks to a month from planning to go-live.
But a large-scale project is a different animal altogether. If you’re trying to untangle multiple legacy systems, map messy and inconsistent data formats, and build custom middleware to make it all work, the timeline will naturally stretch. These more involved projects typically take anywhere from 6 to 12 months, and sometimes even longer.
Your project’s timeline will hinge on a few key factors:
-
Number of Systems: The more endpoints you’re connecting, the more complex the web becomes.
-
API Quality: Do your existing systems have modern, well-documented APIs? If not, you’ll need creative (and more time-consuming) workarounds.
-
Data Complexity: The volume and, more importantly, the cleanliness of the data you’re moving and mapping have a huge impact on the schedule.
-
Testing Depth: When you’re dealing with clinical data, you can’t afford to rush testing. This phase is non-negotiable and needs the time it deserves.
A thorough discovery and planning phase upfront is the only way to lock in a realistic and achievable timeline.
What Are the Biggest Roadblocks in EHR Integration?
Every integration project has its own unique quirks, but we see the same few hurdles pop up time and time again. A good partner will help you see these coming and navigate them before they derail your project.
Here are three of the most common obstacles you’ll likely face:
-
Semantic Interoperability: This goes way beyond just moving data from point A to point B. It’s about ensuring everyone agrees on what the data means. For example, does “blood pressure reading” in one system use the same units and definitions as another? Getting this shared understanding right is critical for patient safety and is often the hardest part of the puzzle.
-
Legacy System Handcuffs: Many healthcare organizations are still running on older systems that were built long before the idea of open data exchange was a priority. These systems often lack APIs, use proprietary data formats, and require some serious technical creativity to integrate. Tackling these requires a partner with deep experience in custom software development.
-
Getting Everyone on the Same Page: An integration project touches nearly everyone: clinicians, nurses, IT staff, and billing administrators. Making sure every stakeholder group is aligned on goals, workflows, and priorities is absolutely essential. Without a single, unified vision, projects often get bogged down in conflicting requirements and a lack of clear direction.
Overcoming these challenges isn’t just about technical skill; it requires deep industry knowledge and rock-solid project management. If you plan for these roadblocks from the start, you’ll have a much smoother road to success.
Ready to build a connected healthcare ecosystem that improves outcomes and drives efficiency? As a proven AI solutions partner, Bridge Global combines deep healthcare expertise with advanced technology to deliver robust and scalable EHR integration solutions. We help you unlock the full potential of your data and create a truly interoperable future.



