Your Guide to Modern Healthcare IT Solutions
Healthcare IT solutions are the specialized software, systems, and technologies built to manage health information and automate how healthcare works. These tools, from electronic health records to AI-powered diagnostic platforms, are the digital backbone of modern medicine. They’re what make care more efficient, secure, and truly centered on the patient.
The Digital Heartbeat of Modern Medicine
Picture a hospital where a patient’s information flows instantly and securely between the emergency room, the lab, and the specialist’s office. Imagine intelligent algorithms helping doctors spot potential issues faster, and patients receiving follow-up care from the comfort of their own homes. This isn’t a futuristic vision; it’s the reality that modern healthcare IT solutions are creating right now.

This digital shift is a direct response to some of the industry’s biggest headaches. We’re talking about rising operational costs, a maze of complex regulations, and the high expectations of today’s patients. Technology provides the framework for building a more resilient and responsive health system. At its heart, it’s about using data and connectivity to make healthcare smarter.
Why This Transformation Matters Now
The move toward better digital tools isn’t just a trend; it’s a critical need. We’re dealing with an explosion of health data and constant pressure for greater efficiency. The global healthcare IT market tells the story. Valued at roughly $354 billion in 2025, it’s expected to climb to an astonishing $1,380.51 billion by 2034. That massive investment reflects a clear industry-wide push to improve care delivery through technology. You can dig into the complete market analysis on Fortune Business Insights.
This guide is your practical roadmap to navigating this world. We’ll break down the core pillars of this digital ecosystem, focusing on how to build systems that are advanced, secure, interconnected, and always focused on the patient.
Think of healthcare IT not as a box of separate tools, but as a living, interconnected ecosystem. Each solution, from an EHR to a telehealth app, should work together to paint a complete and actionable picture of patient health.
The Pillars of a Modern Health System
To really get a handle on healthcare IT, you need to understand its key components. These are the foundational technologies that organizations depend on to run smoothly and deliver great care.
-
Data Management & Records: At the center are systems like Electronic Health Records (EHRs) that digitize patient histories, creating a single, reliable source of information.
-
Care Delivery Platforms: Telehealth and remote monitoring tools are breaking down the walls of the clinic, extending the reach of care directly into patients’ homes.
-
Intelligent Analytics & AI: Artificial intelligence and machine learning comb through massive datasets to help predict health outcomes and tailor treatments to the individual.
-
Security & Compliance: None of this works without robust security measures to protect sensitive patient data and ensure everything complies with regulations like HIPAA.
When these pillars work together, they create a powerful synergy, turning isolated data points into coordinated, intelligent healthcare.
What Are the Core Healthcare IT Solutions?
To get a real handle on modern healthcare, you have to understand the technology that underpins it. These core healthcare IT solutions aren’t just fancy software; they’re the interconnected systems that are fundamentally changing how care is delivered. Think of them less like individual tools and more like an integrated nervous system for a hospital or clinic.
Let’s walk through the key pieces of this ecosystem, starting with the very heart of patient data and moving outward to how care is delivered and measured. Each solution solves a specific, real-world problem, and together, they build the foundation for a smarter, more connected healthcare system.
Comparing Core Healthcare IT Solutions
To start, it helps to see how these core solutions fit together. Each one has a distinct role, but they are most powerful when they work in concert. This table gives you a quick snapshot of the “what,” “why,” and “how” for each major category.
| Solution Type | Primary Function | Key Business Benefit | Example Use Case |
|---|---|---|---|
| EHR / EMR | Centralizes all patient health information into a single digital record. | Improves clinical decision-making, reduces errors, and increases operational efficiency. | A doctor instantly pulls up a new patient's complete allergy and medication history. |
| Interoperability | Enables different software systems to securely exchange and interpret health data. | Enhances care coordination across different providers and improves patient safety. | An ER system automatically pulls records from a patient's primary care physician's EHR. |
| Telehealth | Delivers clinical services remotely using telecommunications technology. | Expands access to care, improves patient convenience, and reduces healthcare costs. | A patient in a rural area has a video follow-up appointment with a specialist in the city. |
| IoT / RPM | Uses connected devices to monitor patients' health outside of the clinical setting. | Enables proactive chronic disease management and reduces hospital readmissions. | A smart glucose meter sends a patient's blood sugar readings directly to their care team. |
| Analytics & BI | Processes vast amounts of health data to uncover insights and trends. | Optimizes clinical outcomes, streamlines operations, and informs strategic planning. | A hospital analyzes admission data to better predict staffing needs for the flu season. |
| AI / Machine Learning | Applies advanced algorithms to automate tasks and predict health outcomes. | Increases diagnostic accuracy, personalizes treatment, and automates administrative work. | An AI algorithm analyzes medical images to detect early signs of disease missed by the human eye. |
| Security & Compliance | Protects sensitive patient data and ensures adherence to regulations like HIPAA. | Mitigates risk of data breaches, avoids hefty fines, and builds patient trust. | Encrypting all patient data both at rest and in transit to prevent unauthorized access. |
As you can see, these aren’t just abstract concepts. They are practical tools that solve tangible problems for providers and patients every single day.
Electronic Health Records: The Digital Story of a Patient
At the center of it all is the Electronic Health Record (EHR). Don’t let the clinical name fool you; an EHR is essentially the living, digital biography of a patient’s health. It pulls everything: lab results, medications, imaging, allergies, treatment plans, into one secure, organized place.
Gone are the days of deciphering a doctor’s handwriting or waiting for a paper chart to be wheeled down from another floor. With an EHR, a clinician gets a complete picture of a patient’s history in seconds. That immediate access is absolutely crucial for making the right call, preventing dangerous medical errors, and keeping the entire care team on the same page.
But a modern EHR is more than just a digital filing cabinet. It’s an active partner in care. It can automatically flag a risky drug interaction, send reminders for preventive screenings, and give hospitals the hard data they need to see what’s working and what isn’t. It’s the single source of truth that nearly every other digital tool relies on.
Interoperability: The Universal Language of Health Data
If an EHR is a patient’s story, interoperability is the universal translator that lets everyone read it. In simple terms, it’s the ability for different software systems, even from competing vendors, to talk to each other, share data, and actually understand what that data means.
Without it, a patient’s information is stuck in a digital silo, trapped within the walls of one hospital or clinic. Picture a patient being rushed to an ER while on vacation. With true interoperability, the emergency physician can securely pull up that patient’s full medical history from their doctor back home in a matter of seconds. That means knowing about a life-threatening allergy or a chronic condition instantly.
Interoperability isn’t just about connecting software; it’s about connecting care. It’s the invisible thread that ensures the right information gets to the right person at the right time, no matter where it was created. This seamless data flow is a non-negotiable for patient safety.
Telehealth and Remote Monitoring: The Digital Front Door
Telehealth platforms went from being a “nice-to-have” to an essential part of healthcare almost overnight. These solutions create a “digital front door,” giving patients a way to see their doctor for consultations, follow-ups, or therapy sessions without ever leaving home. This has been a game-changer for access, especially for people in rural areas or for those who have trouble traveling.
Hand-in-hand with telehealth is remote patient monitoring (RPM), which is powered by the Internet of Things (IoT). This is where connected medical devices come into play, allowing care teams to keep an eye on patients’ vitals from afar.
We’re talking about things like:
-
Smart glucose monitors that automatically upload readings for a diabetes specialist to review.
-
Connected blood pressure cuffs that can alert a nurse if a patient’s readings are trending dangerously high.
-
Wearable sensors that track heart rate and oxygen levels for patients recovering from surgery at home.
This steady stream of real-world data allows clinicians to step in before a small problem becomes a crisis. It’s a huge step away from reactive sick-care toward truly proactive healthcare.
Analytics and Business Intelligence: Turning Data into Insight
Every single day, healthcare organizations are flooded with a tsunami of data. Health analytics and business intelligence (BI) are the tools that make sense of it all, turning raw numbers into insights you can actually use. They comb through information from EHRs, billing systems, and patient feedback to spot patterns and predict what’s next.
For instance, a hospital can use analytics to accurately forecast ER visits during flu season, making sure they have enough staff on hand. A health system can analyze patient outcomes across thousands of cases to pinpoint which surgical protocol leads to the fastest recovery. This data-driven thinking is essential for boosting both the quality of care and the financial health of the organization.
How AI Is Reshaping Patient Care
Artificial intelligence isn’t just a futuristic concept anymore. It’s actively working in clinics and hospitals right now, serving as a powerful co-pilot that helps make healthcare smarter, faster, and far more predictive. Think of AI and machine learning as the engines driving real advancements in patient care, moving well beyond simple task automation to genuinely enhance the skills of medical professionals.

At its core, this shift is all about using sophisticated algorithms to spot patterns and insights buried in massive health datasets. The goal is to produce tangible results, from highly personalized treatment plans to more efficient hospital workflows, that ultimately lead to better outcomes for patients.
Enhancing Diagnostic Accuracy
One of the most powerful and immediate impacts of AI is in medical imaging. It’s like giving a radiologist a second set of incredibly sharp eyes. These algorithms can analyze MRIs, CT scans, and X-rays with remarkable precision, often catching subtle indicators of disease that the human eye might overlook.
For instance, an AI model trained on thousands of mammograms can flag suspicious areas with a high probability of being cancerous, prompting the radiologist to focus their attention there. It doesn’t replace the expert’s judgment; it supercharges it, paving the way for earlier, more accurate diagnoses when treatment is most effective. This ability is a true cornerstone of modern healthcare IT solutions.
“AI in diagnostics is less about machine versus human and more about machine with human. It’s a collaborative intelligence that elevates a clinician’s ability to detect disease, interpret complex data, and act decisively, ultimately saving lives.”
Predictive Analytics for Proactive Care
Beyond diagnostics, AI’s real magic lies in its ability to look ahead. Predictive analytics models sift through patient data: from EHRs, wearables, and even genetic profiles, to forecast potential health risks. This capability allows care teams to finally move from a reactive “wait-and-see” approach to a truly proactive one.
Imagine a system that alerts clinicians that a specific patient is at high risk of developing sepsis or having a heart attack within the next 48 hours. By flagging these individuals, doctors and nurses can intervene with preventative measures, dramatically improving outcomes and avoiding costly emergency care.
This forward-thinking approach extends to public health as well. AI models can analyze population data to predict disease outbreaks, helping officials allocate resources more effectively and contain health crises before they spiral out of control.
Streamlining Operations with Intelligent Automation
The administrative load in healthcare is staggering, and it eats up time that clinicians should be spending with patients. This is where generative AI and intelligent automation are stepping in to make a huge difference by handling repetitive yet critical tasks.
-
Automated Clinical Documentation: AI tools can now listen to a doctor-patient conversation and automatically generate clinical notes, summaries, and even billing codes.
-
Optimized Scheduling: Machine learning algorithms can analyze patient flow, surgeon availability, and operating room usage to build incredibly efficient schedules.
-
Intelligent Prioritization: AI can help triage patient messages and administrative requests, ensuring that the most urgent needs are handled first. You might be interested in exploring how AI chatbots are being applied in healthcare.
This kind of automation frees up skilled professionals to focus on the human side of medicine: delivering compassionate, high-quality care. For a deeper look at specific tools, like those for improving patient communication, it’s worth exploring the landscape of AI-powered healthcare communications solutions.
This focus on AI is backed by serious investment. In 2025, AI is a major trend, with the U.S. accounting for 63% of the $279.5 billion global healthcare IT spend. Providers are leading the charge (63.40% of the investment) as they adapt to new interoperability rules, and cloud systems are only amplifying AI’s impact. As a clear example of this efficiency, AI-driven imaging systems have been shown to cut radiologist read times by an average of 23%.
Building a Fortress Around Patient Data
In healthcare, we’re not just dealing with data points; we’re handling people’s lives, their privacy, and their deepest vulnerabilities. That’s why security isn’t just a feature of healthcare IT solutions; it’s the bedrock. Protecting patient data is a fundamental patient safety issue that directly shapes trust and the quality of care.
The consequences of getting this wrong are staggering. The healthcare industry remains a top target for cyberattacks, and the average cost of a breach has climbed to an eye-watering $11 million. To truly grasp the gravity of the situation, it’s worth understanding the full spectrum of risks of HIPAA non-compliance – the stakes couldn’t be higher.
Moving Beyond Compliance Acronyms
It’s easy to get lost in the alphabet soup of regulations like HIPAA in the United States or GDPR in Europe. But if you strip away the jargon, their purpose is simple and powerful: to protect a patient’s most sensitive information from falling into the wrong hands.
Building compliant software is about more than just ticking boxes on a checklist. It demands a security-first mindset right from the project’s inception. This means designing systems where patient privacy is the default, not an add-on. For a practical look at what this entails, our guide on HIPAA-compliant software development breaks down the process.
A solid security strategy hinges on a continuous, multi-step process.
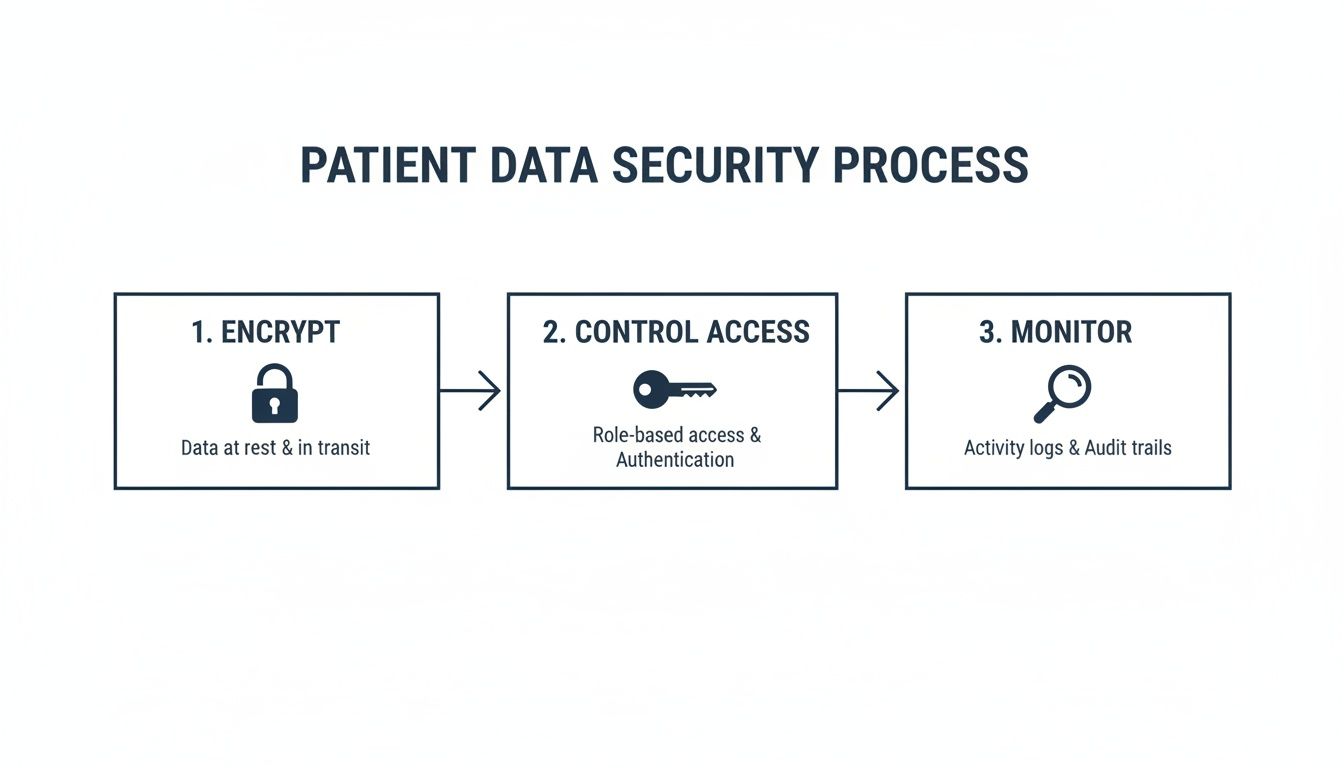
As you can see, robust security isn’t a one-and-done setup. It’s a perpetual cycle of encrypting data, controlling who can see it, and constantly monitoring for threats.
Essential Defense Strategies
Effective data protection is a multi-layered game, defending against both sophisticated external attacks and simple internal mistakes. Today’s threats are diverse, from ransomware that can paralyze an entire hospital to accidental data leaks by well-meaning staff.
To build a proper defense, every secure health tech solution must be built on three core pillars:
-
Robust Encryption: This is your digital lockbox. Data must be encrypted both “at rest” (while sitting on a server) and “in transit” (as it moves across the network). It essentially scrambles sensitive information into an unreadable code that only authorized people can unlock.
-
Strict Access Controls: Not everyone in a clinic or hospital needs to see every piece of patient data. Role-based access control (RBAC) enforces the “principle of least privilege,” ensuring users can only view and edit the information absolutely required for their job. This one practice drastically shrinks the risk of exposure.
-
Continuous Security Monitoring: Cyber threats are constantly evolving, so your defenses must too. This means using smart tools to watch for suspicious activity, running regular security audits, and actively hunting for weaknesses before they can be exploited by attackers.
A secure system isn’t a barrier to progress; it’s the very foundation upon which patient trust is built. A secure solution is an effective solution.
Choosing and Implementing Your Solution
Picking the right healthcare IT solution is just the start. The real challenge, and where the value is truly created, is weaving that technology into the very fabric of your organization. A successful rollout isn’t a one-off event; it’s a carefully orchestrated process that has to balance powerful technology with the realities of human workflows.
This is what separates a tool that gathers dust from one that genuinely improves patient outcomes and makes your operations more efficient. It all comes down to having a clear, pragmatic roadmap. From defining what you actually need to vetting vendors and managing the launch, every step counts. The goal isn’t just to install new software; it’s to deliver tangible, measurable value to your clinicians, staff, and patients.
Laying the Groundwork with a Needs Analysis
Before you even think about looking at a vendor demo, you have to start with a deep and brutally honest needs analysis. This isn’t just about spotting a problem; it’s about defining its precise shape, size, and impact. Jumping into sales calls without this clarity is like shopping for a cure without a diagnosis; you’ll get dazzled by flashy features that don’t solve your root problem.
Start by asking the hard questions:
-
What specific workflow is broken? Is it the patient intake process, the way clinicians document encounters, or the billing cycle? Be specific.
-
Who feels the pain most? You need to talk directly to the nurses, doctors, administrators, and even patients who are living with the problem every day.
-
What does “better” look like? Are you trying to cut patient wait times by 15%? Or maybe your goal is to eliminate administrative errors or improve how different departments share information.
This process gives you a detailed blueprint of your real requirements. It becomes your north star, guiding every decision you make and keeping you from getting sidetracked by tech that doesn’t serve your core mission.
A thorough needs analysis transforms your procurement process from a feature-driven shopping trip into a strategic, problem-solving mission. It ensures the solution you choose is the one you actually need.
How to Evaluate Potential Vendors
Once you have your requirements locked down, you can start evaluating vendors. This stage demands a critical eye and a structured approach to cut through the marketing fluff and see which partners can deliver on the metrics that truly matter. A slick user interface is great, but it’s the underlying architecture and the quality of support that will determine your long-term success.
Your evaluation checklist should be built around a few non-negotiables.
-
Interoperability and Integration: Any new solution has to play well with your existing tech stack. Ask for concrete examples of how their system integrates with your EHR, billing platforms, and lab systems using modern standards like FHIR APIs. If a vendor can’t or won’t connect with other systems, it’s a massive red flag.
-
Scalability and Future-Readiness: Your organization is going to evolve, and your technology needs to keep pace. You should be asking about their product roadmap. For healthcare organizations aiming for agility, understanding a vendor’s approach to the cloud is a must. You can learn more by exploring the key steps in planning a successful healthcare cloud transformation.
-
Security and Compliance: This is absolutely non-negotiable. The vendor must have a rock-solid track record of upholding HIPAA standards and deploying robust data protection. Ask to see documentation on their security protocols, data encryption methods, and breach response plans.
-
Training and Ongoing Support: The most brilliant software is worthless if your team can’t use it effectively. Dig into the quality of their training programs and find out how responsive their customer support is. Better yet, ask for references and talk to their current clients to get the real story on their post-launch partnership.
Strategies for a Phased and Successful Rollout
Finally, we get to the implementation itself. A “big bang” launch, where the new system goes live for everyone all at once, is often a recipe for chaos and can seriously disrupt clinical care. A phased rollout is almost always the smarter, safer bet. This means introducing the solution to one department or a small group of users at a time.
This methodical approach lets you gather real-world feedback, fix bugs on a small scale, and cultivate a group of internal champions who can help train and support their colleagues. It turns a daunting, high-risk project into a manageable series of small wins.
To really nail the rollout, focus on user adoption from day one. Get your clinical staff involved in the final configuration and testing phases so the system is shaped to fit their needs, not the other way around. Clear communication, good training, and celebrating small victories will build the momentum you need for a successful, organization-wide deployment.
Healthcare IT Success Stories in Action
It’s one thing to talk about technology in theory, but where the rubber really meets the road is in the real world. To grasp the true power of well-planned healthcare IT solutions, you have to see them in action – solving tough operational problems for providers and, most importantly, changing patients’ lives for the better.
These examples show what happens when the right tech is implemented with a clear purpose.

This is where abstract ideas like interoperability and patient engagement become tangible success stories. Let’s look at a couple of scenarios that highlight how smarter, more connected healthcare benefits real people and organizations.
Expanding Care with Telehealth
Imagine a regional practice with several clinics, constantly battling high no-show rates. For many of their patients, especially those in rural areas, getting to an appointment was a major hurdle. They faced long drives, time off work, and transportation challenges.
The practice decided to tackle this head-on by launching a comprehensive telehealth platform, effectively creating a “digital front door.” Suddenly, patients could handle follow-up visits, medication checks, and even behavioral health sessions through secure video calls from home.
The impact was almost immediate:
-
No-Show Rates Plummeted: Within just six months, missed appointments dropped by a staggering 40%.
-
Access to Care Grew: They were able to bring in dozens of new patients from remote communities who simply couldn’t get to the clinic before.
-
Better Chronic Disease Management: Patients with ongoing conditions could check in more regularly, leading to more consistent and effective care without the hassle of travel.
This is a perfect example of how one smart solution can fix multiple problems at once – boosting efficiency for the clinic while knocking down barriers to care for patients.
Success in healthcare IT is measured by its impact on people. It’s about a rural patient getting specialist advice without a four-hour drive, or a care team preventing a crisis because they had the right data at the right moment.
Optimizing Hospital Operations with AI
Now, think about a busy urban hospital wrestling with a classic bottleneck: operating room (OR) scheduling. The whole system was plagued by last-minute cancellations, wildly inaccurate time estimates for surgeries, and clunky coordination between teams. The result? Expensive surgical suites sat empty, and staff morale was low.
The hospital brought in a technology partner to deploy an AI-driven analytics platform. This system chewed through years of surgical data, everything from procedure types and surgeon-specific timing to equipment usage, and started building incredibly accurate predictive models.
This new, smarter scheduling system completely changed their workflow:
-
Predictive Scheduling: The AI algorithm could forecast the length of each surgery with a high degree of accuracy, allowing for a much tighter and more realistic OR schedule.
-
Smarter Resource Allocation: It automatically assigned staff, rooms, and equipment, ensuring everything was lined up and ready to go, which drastically cut down on idle time.
-
Real-Time Adjustments: The platform could even spot potential scheduling conflicts before they happen and suggest proactive changes, stopping a small delay from turning into a full-blown crisis.
The results were huge, both clinically and financially. The hospital saved millions through better use of its resources and was able to increase the number of surgeries it performed. This data-first approach didn’t just help the bottom line; it also made patients happier by cutting down on long waits and frustrating postponements. These stories prove that the best healthcare IT solutions are never just about the technology itself; they’re about creating better outcomes for everyone.
Got Questions About Healthcare IT? We’ve Got Answers.
Diving into healthcare technology always brings up a few tough, practical questions. When you’re thinking about investing in new systems, concerns about cost, complexity, and how everything will work together naturally rise to the surface. Getting a handle on these common roadblocks is the first step to building a smart plan for any healthcare IT solution.
Let’s tackle some of the most frequent questions we hear from healthcare leaders.
What Is the Biggest Challenge in Implementing a New Solution?
It’s almost never the technology itself; it’s the people. The single biggest hurdle is user adoption and change management. Clinicians, nurses, and administrative staff have deeply ingrained workflows, and dropping a new system into their laps can feel like a major disruption. If the people who need to use the tool every day don’t buy in, even the most sophisticated software is doomed to fail.
A successful rollout depends on three things: a rock-solid communication plan, hands-on training that makes sense for their roles, and, most importantly, involving your clinical teams in the selection process from the start. That’s how you ensure the new system actually makes their lives easier, not harder.
How Can Smaller Clinics and Practices Afford Advanced IT?
The sticker shock can be real, but the game has changed. Many of the best tools are now offered as cloud-based SaaS (Software as a Service) models. This completely sidesteps the need for a massive upfront investment in servers and other hardware. Instead, you pay a predictable monthly or yearly fee, putting powerful EHRs and data analytics tools within reach for smaller providers.
Another smart move is to start with a tailored MVP (Minimum Viable Product). This strategy involves building a solution that solves your most urgent problems first. You get value right away, and you can add more features and capabilities as your organization grows and your budget allows.
The old days of monolithic, one-size-fits-all systems are over. Cloud delivery and MVP development have opened the door for smaller practices to access the same powerful technology as the big players, leveling the playing field.
How Do You Make Sure a New System Will Talk to Your Old Ones?
This is the million-dollar question of interoperability, and it needs to be a non-negotiable requirement when you’re vetting new software. To get your systems talking to each other, you need to look for solutions built on modern standards like FHIR (Fast Healthcare Interoperability Resources). Think of FHIR as a universal translator for health data.
Before you sign any contracts, you have to do your homework. That means a complete audit of your current systems and their APIs. A good technology partner can then map out exactly how data needs to flow and build custom integrations where necessary. This foundational work prevents data from getting stuck in digital silos and ensures a patient’s information can move securely across your entire organization.
At Bridge Global, we don’t just build software; we architect secure, interoperable, and scalable healthcare IT solutions that solve real-world problems. Learn how our AI-driven development process can help you build the right solution for your organization.



