Your Guide to Digital Health Platform Engineering
Digital health platform engineering isn’t just about building another app. It’s the highly specialized work of designing and constructing the technological backbone that ties together all the disconnected pieces of the healthcare puzzle.
Think of it as creating the central nervous system for a hospital or health system. This is the architecture that allows a patient’s portal, the doctor’s electronic health record (EHR), an AI-powered diagnostic tool, and a wearable fitness tracker to talk to each other securely and instantly.
The Blueprint for Modern Healthcare
Where traditional software development often creates standalone solutions for specific problems, platform engineering takes a different route. The goal here is to build a reusable, scalable, and secure foundation that new applications and services can simply plug into. It’s a strategic discipline that lets healthcare organizations innovate quickly without breaking what already works or compromising on security.
This shift isn’t just a trend; it’s a response to enormous market demand. The global digital health market is projected to hit an incredible $549.7 billion by 2028, expanding at a compound annual growth rate of 25% from 2023. That explosive growth shows just how aggressively organizations are moving toward platform-based models for everything from telehealth and data analytics to AI-driven patient care.
The table below breaks down the fundamental pillars that make up a strong digital health platform.
Core Pillars of Digital Health Platform Engineering
| Pillar | Description | Key Engineering Focus |
|---|---|---|
| Interoperability | The ability for different systems—from old-school EHRs to new mobile apps—to exchange data without a hitch. | Implementing data standards like FHIR, building robust APIs, and managing complex data transformations. |
| Security & Compliance | Embedding ironclad protections for sensitive patient data from the very beginning, meeting strict regulations. | Engineering for HIPAA, GDPR, and HITRUST compliance; includes encryption, access control, and continuous monitoring. |
| Scalability | Designing an architecture that can grow with the organization, handling more data, users, and transactions over time. | Using cloud-native services, microservices architecture, and elastic infrastructure to manage demand. |
| Developer Experience | Providing tools, clear documentation, and automated workflows that help developers build and deploy new features quickly. | Creating well-documented APIs, CI/CD pipelines, and internal developer portals (IDPs). |
These components are not just features; they are the essential building blocks for a system that can support the entire patient journey and make clinical operations run smoothly.
Why a Platform Approach Is a Game-Changer
Embracing a platform engineering mindset gives healthcare organizations a serious edge. It lets them move faster, cut down on redundant development work, and offer a reliable, secure experience for both patients and clinicians.
By investing in a solid foundation, an organization can stop reinventing the wheel and start focusing on high-impact services. Think predictive analytics that can spot disease risks early or personalized tools that keep patients engaged in their own care. As we explored in our guide, the principles of software engineering in healthcare are critical for building systems that are both powerful and sustainable. Ultimately, this strategic approach is what will power the next generation of patient care.
Designing a Future-Proof Platform Architecture
When you’re building a digital health platform, think of it like building a hospital. You could go the old-school route and construct a single, massive building where every department is permanently welded together. This is a monolithic design. It works, at first. But what happens when you need to upgrade the radiology wing? You can’t do it without shutting down or disrupting the entire hospital. It’s slow, risky, and incredibly expensive.
This is exactly the problem with outdated architecture in digital health.
A modern, future-proof approach is completely different. It views the platform less like a single building and more like a high-tech campus. On this campus, you have a series of specialized clinics connected by smart, efficient pathways. This is the heart of a microservices architecture. Each core function—patient scheduling, billing, electronic health records (EHR), telehealth—operates as its own independent service.
This modularity is a genuine game-changer. You can update, scale, or even completely replace the “billing clinic” without touching the “EHR clinic.” This kind of agility is essential for continuous innovation and is a hallmark of great custom software development.
The Architectural Cornerstones
To build a platform that can actually evolve, engineers have to focus on a few key principles that bake flexibility and scalability in from the start. Getting these foundational choices right is what prevents the system from becoming a technical dinosaur in just a few years.
- API-First Design: This philosophy treats your Application Programming Interfaces (APIs) as the main event, not an afterthought. You design the APIs first, creating a clear, stable contract for how different microservices will talk to each other. It’s like creating a universal language for all the specialized clinics on your campus, making sure they can coordinate seamlessly.
- Serverless Computing: With this cloud model, you run your code without ever thinking about the underlying servers. For a health platform, this is huge. It means you can automatically scale up to handle a sudden flood of telehealth appointments and then scale back down, only paying for the computing power you actually used. It’s a fantastically efficient way to manage unpredictable demand.
- Event-Driven Architecture: In this setup, services react to “events” as they happen. For example, when a new lab result is ready (the event), the system can automatically ping the doctor’s dashboard and the patient’s portal. This creates a hyper-responsive system where different parts react to real-time information without being rigidly connected.
The diagram below shows how these interconnected pillars come together to support a truly robust platform.
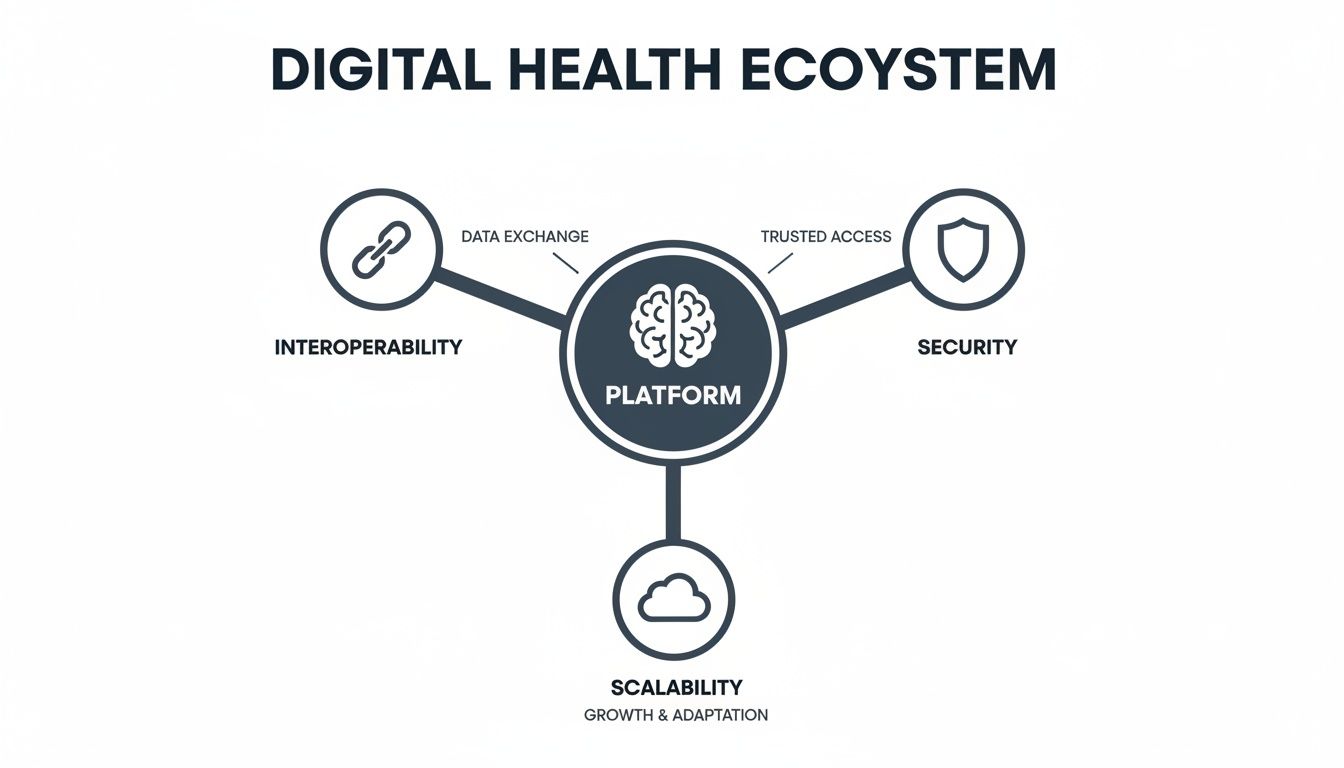
As you can see, a central platform has to nail interoperability, security, and scalability to work as one cohesive, effective system.
Scaling for the Future of Care
The need for this kind of architecture isn’t just a theory; it’s being driven by massive shifts in how patients get care. Just look at telehealth. The global market is on track to explode to an incredible $3.42 trillion by 2028. This kind of growth means platforms must be ready to handle millions of concurrent video calls, connect with thousands of new IoT devices, and maintain perfect security at a massive scale.
A truly future-proof architecture anticipates this growth from day one. It’s not just about meeting today’s needs. It’s about creating a foundation that can absorb tomorrow’s demands without forcing you into a complete, system-wide rebuild.
Building for the future also means adopting more sophisticated security models. A perfect example is the Zero Trust Architecture, a modern security mindset that operates on a simple principle: “never trust, always verify.” It assumes no user or device is safe by default.
By making these smart architectural choices early, you can build a digital health platform that’s truly resilient. This foundation will let you deliver exceptional care today and seamlessly plug in the next wave of health innovations—from advanced AI diagnostics to new forms of virtual care, for years to come.
Building a Fortress of Security and Compliance
In digital health, data security isn’t just a technical box to check—it’s the very foundation of patient trust. A single breach does more than just expose data; it can permanently shatter a patient’s confidence and bury an organization under a mountain of legal and financial penalties. That’s why great digital health platform engineering doesn’t see security and compliance as constraints. Instead, they’re treated as the essential blueprints for building systems that are safe, reliable, and worthy of trust.
Imagine a modern digital health platform not just as a building, but as a high-tech bank vault. You wouldn’t rely on a single thick door. Real security comes from layers of independent, reinforcing defenses that protect sensitive information from every possible angle. This mindset is at the heart of specialized healthcare software development, where the stakes are as high as they get.
Understanding the Regulatory Maze
One of the biggest engineering hurdles is navigating the tangled web of global regulations. While each framework has its own quirks, they all share a common purpose: to protect patient privacy and give people control over their own data.
- HIPAA (Health Insurance Portability and Accountability Act): This is the bedrock of U.S. health data law. It sets the standard for protecting sensitive patient health information (PHI) and dictates exactly who can view, use, or share it.
- GDPR (General Data Protection Regulation): The EU’s comprehensive data privacy law gives individuals sweeping rights over their personal data, including health records. Its reach is global, impacting any company that processes data for EU citizens.
- HITRUST (Health Information Trust Alliance): Think of HITRUST as a unifying framework. It’s a certifiable security standard that helps organizations harmonize requirements from ISO, NIST, HIPAA, and others into a single, cohesive approach to risk management.
A critical piece of the puzzle, especially with today’s technology, is ensuring GDPR compliant AI integration when processing sensitive health data across different countries.

Engineering Security from the Ground Up
You can’t just bolt on compliance at the end of a project. It has to be woven into the very fabric of the platform’s architecture from day one. This “security by design” philosophy turns compliance from a reactive, checklist-driven chore into a proactive, automated strategy that makes the entire system stronger. Building these safeguards is a complex but absolutely non-negotiable part of the job. As we’ve detailed before, mastering the nuances of HIPAA-compliant software development is a must-have skill for any team in this space.
This all comes back to implementing multiple layers of protection, just like our bank vault.
A truly secure system works on the assumption that threats can come from anywhere—both outside and inside the organization. The engineering goal is to shrink the attack surface and ensure that even if one layer is breached, others stand ready to contain the threat and stop a catastrophic data loss.
This proactive mindset depends on a set of essential engineering practices that form the pillars of a secure platform.
A Practical Security Checklist for Engineers
Turning compliance theory into solid engineering practice takes a systematic approach. Here’s a foundational checklist for building a digital health platform that’s both secure and compliant.
- End-to-End Encryption: Data must be encrypted everywhere, all the time. That means it’s encrypted at rest (while sitting in a database) and in transit (as it moves over a network). If data is ever intercepted, it’s just unreadable gibberish.
- Granular Access Controls: Implement Role-Based Access Control (RBAC) to live by the Principle of Least Privilege. In plain English, a nurse should only be able to access the specific patient data they need for their job—and absolutely nothing more.
- Immutable Audit Trails: Every single action involving patient data – every view, every edit, every share -must be logged in a tamper-proof audit trail. This is your source of truth for accountability and for investigating any potential incidents.
- Regular Vulnerability Scanning and Penetration Testing: You have to proactively hunt for weaknesses. Automated scanning and “ethical hacking” exercises are crucial for finding and fixing vulnerabilities before bad actors can find them.
- Secure Software Development Lifecycle (SSDLC): Security can’t be an afterthought. It needs to be part of every stage of development, from the initial design and coding to testing and deployment. This includes things like static code analysis, dependency scanning, and mandatory secure coding training for all developers.
By embedding these principles directly into the engineering workflow, you can build platforms that aren’t just powerful and innovative, but are also deserving of the immense trust patients place in them.
Integrating AI and Achieving True Interoperability
A digital health platform’s real value emerges when it stops being a passive data warehouse and starts actively using that data to make smart decisions. This is where artificial intelligence (AI) and genuine interoperability come together, turning a basic system into a dynamic powerhouse that can predict health risks, tailor patient care, and automate tedious clinical tasks. This intelligence layer is the secret sauce.
But here’s the catch: AI is only as smart as the data it’s fed. If your platform’s data is trapped in isolated silos, an EHR that won’t talk to the pharmacy system, or a wearable device that can’t sync with a patient’s record, your AI’s potential is completely hamstrung. It’s like trying to run a Formula 1 car on a few drops of low-grade fuel. True interoperability isn’t a “nice-to-have”; it’s the absolute foundation for any meaningful AI integration.
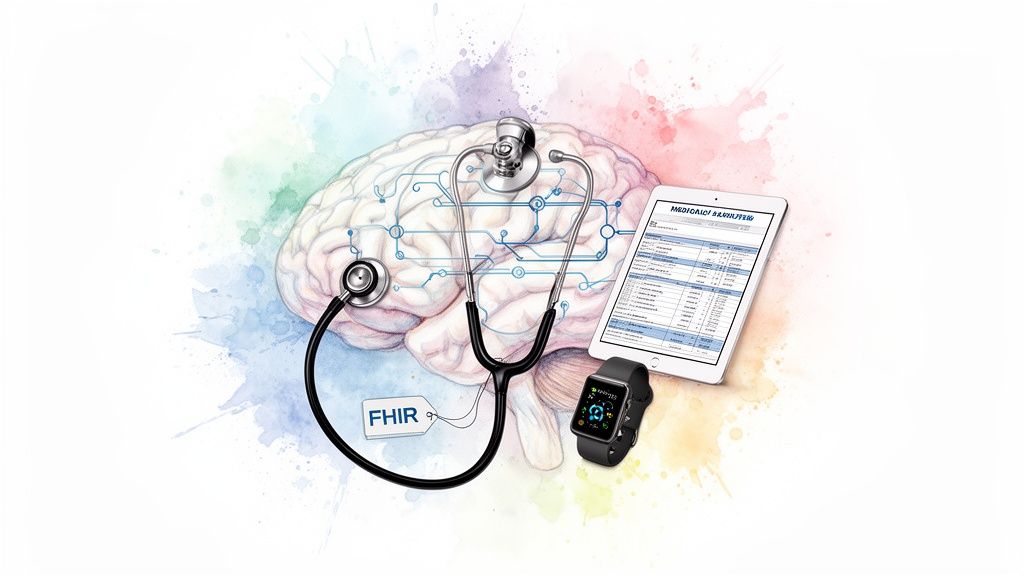
Why FHIR is the Universal Translator for Health Data
For years, getting different healthcare systems to communicate has been a massive headache. They all speak different languages and structure data in unique ways, making any attempt at connection a complex, custom-coded nightmare. This is exactly the problem that modern standards like FHIR (Fast Healthcare Interoperability Resources) were designed to fix.
Think of FHIR as a universal translator for health data. It doesn’t force every system to be the same; instead, it provides a common language they can all use to talk to each other. It uses modern, web-based APIs to define a shared set of “resources”—like ‘Patient’, ‘Observation’, and ‘MedicationOrder’ that are universally understood.
By adopting FHIR, a platform can finally build seamless data pipelines connecting all the disparate pieces of the puzzle:
- Electronic Health Record (EHR) systems
- Wearable gadgets and IoT sensors
- Pharmacy and laboratory information systems
- Patient-facing mobile apps
This free-flowing, unified data stream is the bedrock of modern digital health platform engineering. It guarantees that when an AI model needs to analyze a patient’s full health history, it gets a complete, coherent story, not a jumble of disconnected fragments. As an experienced AI solutions partner, we see this every day—designing these critical data pipelines is the first step to fueling powerful machine learning models.
From Data Access to Predictive Power
With true interoperability in place, a platform can finally start putting its data to work in some incredible ways. And the market is taking notice. The healthcare data industry is expected to grow by up to 39% annually over the next decade. Meanwhile, AI-driven digital health is projected to rocket from $15.1 billion in 2022 to $187.9 billion by 2030.
This explosive growth isn’t just hype; it’s driven by real-world results. Once you have access to rich, interconnected data, you can build AI-powered features that were impossible before. For example, we help our partners build models that can:
- Predict Disease Risk: Sift through patient data to flag individuals at high risk for conditions like sepsis or heart failure, giving clinical teams a chance to intervene early.
- Personalize Treatment Plans: Combine genetic, lifestyle, and clinical data to recommend the most effective treatments for each unique patient.
- Automate Clinical Documentation: Use Natural Language Processing (NLP) to turn a doctor-patient conversation into perfectly structured clinical notes, freeing up hours of a clinician’s time.
- Optimize Hospital Operations: Forecast patient admission rates to help hospitals manage bed capacity and staff schedules more effectively.
Healthcare Interoperability Standards Comparison
While FHIR is leading the charge, it’s helpful to understand the landscape of standards that have shaped health data exchange. Each was built for a different era and has its own strengths.
| Standard | Primary Use Case | Data Format | Key Advantage |
|---|---|---|---|
| HL7 v2 | Traditional clinical data exchange (admissions, orders) | Pipe-and-hat delimited text | Widespread adoption in legacy systems |
| CDA | Clinical document exchange (discharge summaries) | XML | Provides rich clinical context in a document-centric way |
| DICOM | Medical imaging (X-rays, MRIs) | Binary | The global standard for transmitting and storing images |
| FHIR | Modern, API-based data access for web & mobile | JSON, XML | Flexible, developer-friendly, and built for the modern web |
Understanding these standards helps in planning migrations and ensuring your platform can communicate with both modern and legacy systems, but for new development, FHIR is almost always the way forward.
Interoperability provides the data, and AI provides the intelligence. A successful digital health platform must master both. It’s not about choosing one over the other; it’s about engineering a system where seamless data exchange directly enables smarter, more predictive healthcare.
As you map out your platform’s future, it’s critical to think about these two elements from day one. We dive deeper into this in our detailed look at AI’s expanding role in healthcare. By engineering for both interoperability and AI from the start, you can build a platform that doesn’t just solve today’s problems but is ready to deliver the next generation of intelligent, data-driven patient care.
Breathing New Life into Old Systems, Without Skipping a Beat
A lot of healthcare organizations are running on IT systems that are, to put it mildly, showing their age. These legacy platforms can be decades old, acting as the digital backbone for critical operations. But they’re also like a historic building with ancient wiring—you can’t just rip it all out without a plan, especially when patient care is on the line.
The very idea of a “rip and replace” project is enough to cause nightmares for any CIO. The fear of shutting down essential services for weeks or months is very real.
But modern digital health engineering isn’t about demolition. It’s more like a careful, strategic renovation. The goal is to upgrade the infrastructure piece by piece, all while the daily business of caring for patients continues without a hitch.
The first step is always a frank assessment of what you have. You need to map out the entire technology stack, identifying which parts are the most fragile, where the most critical data lives, and what poses the biggest security threat. This audit becomes your blueprint for a targeted modernization effort.
A Step-by-Step Modernization Plan
Trying to swap out an entire legacy system in one massive project is almost always a recipe for failure. A much smarter—and safer—approach is to do it gradually, piece by piece. This strategy dramatically lowers the risk and lets your organization see the benefits at every stage.
Here’s how that usually works:
- Step 1: Isolate and Wrap It. The first move is to build a modern API layer that sits on top of the old system. Think of it as a protective shell. This allows new, modern applications to talk to the legacy core through a secure, standardized translator, without ever having to touch the fragile code directly.
- Step 2: Apply the Strangler Fig Pattern. It sounds dramatic, but this is a brilliant technique. You strategically build new microservices to take over specific functions from the old system. Over time, these new services slowly and safely “strangle” the legacy application until it’s no longer needed and can be retired.
- Step 3: Migrate Data Strategically. In healthcare, data is everything. Any successful modernization project depends on a meticulously planned data migration. This often means moving information from old on-premise servers to a secure, compliant cloud platform, which opens up a world of possibilities for advanced analytics and AI.
Modernizing a legacy health system isn’t a single, monolithic project. It’s a series of controlled, deliberate steps. The whole point is to de-risk the process by breaking it into manageable phases, ensuring that clinical workflows and patient care are never, ever compromised.
The Power of Cloud and DevOps
This kind of gradual upgrade is made infinitely easier with cloud infrastructure and DevOps practices. The cloud gives you the flexible, scalable environment you need to build and test new microservices without having to buy and set up a mountain of new hardware first.
At the same time, putting a Continuous Integration and Continuous Deployment (CI/CD) pipeline in place automates much of the testing and deployment process. This means every new component of your modernized platform is rigorously checked for security flaws and bugs before it goes live, allowing you to iterate quickly and safely.
Pulling off this kind of complex transition often means bringing in a partner who truly understands both the old world of legacy systems and the new world of modern architecture. An experienced AI solutions partner can offer the strategic guidance and technical firepower needed to make it all happen smoothly. By combining proven modernization patterns with solid custom software development, organizations can finally break free from the shackles of outdated tech.
The payoff is huge: better security, more agility, and the ability to plug in the latest digital health tools. To see what this looks like in the real world, you can check out some of our successful client cases and learn how we’ve helped organizations navigate this exact journey.
Choosing the Right Engineering Partner
Building a digital health platform isn’t something you can just outsource to any software shop. The success of the entire project really comes down to the team you choose to build it with. This isn’t about finding a vendor; it’s about forging a strategic alliance with a partner who gets the immense pressure and unique complexities of healthcare.
Choosing the right team means looking past pure technical talent. You need a partner who can offer genuine strategic guidance, guarantee compliance isn’t an afterthought, and fully support your vision for the long haul. A great partner doesn’t just write code, they bring a consultative mindset, helping you strike that difficult balance between innovating quickly and meeting the non-negotiable demands of healthcare regulations.
Core Competencies to Look For
When you start vetting potential partners, some skills are simply table stakes. Your engineering ally has to bring proven, hands-on experience in the specific domains that make or break healthcare technology. This is the only way to ensure they can build a platform that’s not just working, but also secure, scalable, and ready for whatever comes next.
Here’s a quick checklist of what to look for:
- Deep Regulatory Knowledge: They need to be fluent in HIPAA, GDPR, and HITRUST. Ask to see their portfolio; it should be full of projects that prove they know how to build compliant systems from day one.
- Scalable Architecture Skills: Look for a deep bench of experience with microservices, cloud-native development, and API-first design. This is crucial for building a platform that can handle growth without crumbling.
- Proven AI and Data Expertise: A demonstrated track record is key. They should be able to show you how they’ve built data pipelines and put machine learning models to work for real healthcare scenarios. This is where an expert in AI development services can be a game-changer.
Beyond the Checklist: Finding a Strategic Ally
A true technology partner becomes a seamless extension of your own team. They should be comfortable challenging your assumptions, offering fresh strategic insights, and helping you anticipate problems before they happen. That kind of proactive thinking is what separates a decent vendor from a truly great partner.
The right partner doesn’t just build what you ask for; they help you build what you need. They understand that successful healthcare software development is about creating lasting value, not just checking boxes on a short-term project.
An experienced AI solutions partner can put your roadmap on the fast track, showing you how to use AI for your business to create a real competitive edge. By picking a partner who truly understands the nuances of custom software development in a tightly regulated space like healthcare, you’re setting your organization up for success that lasts.
Frequently Asked Questions
When you’re deep in the weeds of building healthcare technology, questions are inevitable. Here are some straightforward answers to the common questions we hear from leaders and engineering teams navigating digital health platform development.
What’s the Single Biggest Hurdle in Digital Health Platform Engineering?
It really boils down to a fundamental tension: the need to innovate quickly versus the absolute necessity of airtight security and compliance. You’re trying to build a platform that can incorporate sophisticated AI and deliver a fantastic user experience, but you have to do it all while meeting every letter of regulations like HIPAA.
This creates a real balancing act. You can’t just move fast and break things when patient data is on the line. It demands a unique engineering culture that marries agility with a deep, almost obsessive focus on protecting sensitive information. That’s why working with a skilled AI solutions partner who already understands this dynamic can make all the difference.
How Do Microservices Actually Help a Digital Health Platform?
Think of a microservices architecture as breaking down a huge, monolithic application into a collection of smaller, independent parts. In a health platform, this means your appointment scheduling feature can be updated, tweaked, or fixed without ever affecting the core electronic health record system.
The practical benefits here are huge:
- Smart Scaling: If your patient portal gets a surge in traffic, you can scale just that service instead of the entire application. It’s far more efficient.
- Built-in Resilience: If one component fails—say, the billing service has a glitch—it doesn’t bring down the whole system. For healthcare, that uptime is critical.
- Faster Innovation: Your teams can work on different services independently, deploying updates and new features much faster and with less risk.
This modular approach is a cornerstone of modern custom software development, and it’s especially powerful in a complex domain like healthcare.
Can We Really Add AI to Our Old Legacy Healthcare System?
Yes, you absolutely can. The key is to be strategic, this isn’t about ripping and replacing your entire infrastructure overnight. A much smarter path is to use modern tools like middleware and APIs to act as a bridge.
You can essentially create a secure data pipeline that feeds information from your legacy system to a new, powerful AI engine. This lets you tap into years of valuable patient data for things like predictive health analytics or automating clinical workflows, all without disrupting the daily operations that rely on the old system. As we’ve detailed in our guide on the role of AI in healthcare, this kind of phased modernization is almost always the best way to go.
What’s the Big Deal with FHIR in Modern Health Platforms?
In simple terms, FHIR (Fast Healthcare Interoperability Resources) is the universal translator for health data. Its entire purpose is to create a common language that allows completely different systems to talk to each other. A hospital’s EHR, a patient’s wearable device, and a diagnostic lab’s software can finally exchange information without a hitch.
For any modern digital health platform, adopting FHIR isn’t just a good idea, it’s essential. It’s what makes true data fluidity possible, which is the foundation for everything from coordinated patient care to large-scale population health analysis.
Ready to build a secure, scalable, and intelligent digital health platform? The expert teams at Bridge Global specialize in AI-driven healthcare software development that meets the highest standards of compliance and innovation. Partner with us to accelerate your digital health roadmap.