A Guide to Healthcare Data Interoperability Services
Think of healthcare data interoperability services as the universal translator for the healthcare industry. They’re the technology and processes that allow completely different health systems like your hospital, your primary care doctor’s office, and a specialist lab to securely share, understand, and actually use patient information.
This connection creates a single, comprehensive view of a patient’s health journey. It’s absolutely critical for improving the quality of care, slashing medical errors, and bringing down operational costs. In simple terms, it makes healthcare work better for everyone. Explore smarter healthcare tech solutions that take care of data interoperability.
Why Connected Healthcare Data Is No Longer Optional
Imagine trying to solve a complex puzzle with half the pieces missing. That’s what doctors and nurses face every single day when dealing with fragmented patient data. A person’s medical story is often scattered across dozens of different hospitals, clinics, and labs, creating a broken narrative that can put their health on the line.
Healthcare data interoperability is the thread that ties all that scattered information together into one coherent story. It’s far more than just a technical buzzword; it’s the very backbone of modern, effective healthcare. Without it, clinicians are forced to make crucial decisions with an incomplete picture, which can have serious consequences.
The Real-World Costs of Data Silos
When health systems can’t talk to each other, patients and providers feel the pain directly. This lack of a connected data network creates dangerous blind spots and frustrating inefficiencies.
- Redundant and Costly Tests: How many times has a patient had to repeat a blood test or an X-ray just because their new doctor couldn’t get the results from the last one? It happens constantly.
- Critical Diagnostic Delays: A complete medical history is the key to an accurate diagnosis. When pieces are missing, it can delay the identification of serious conditions and compromise treatment.
- Increased Risk of Medical Errors: An incomplete list of medications or allergies is a recipe for disaster, potentially leading to harmful prescription errors or adverse drug reactions.
These data gaps are a direct threat to patient safety and a massive source of wasted spending in healthcare. Working with an expert AI solutions partner can help organizations build the digital bridges needed to tear down these silos and deliver a higher standard of care.
A truly connected healthcare system ensures that a patient’s complete medical history is available at the point of care, empowering clinicians to make the best possible decisions with confidence and clarity.
The Global Push for Connectivity
The need for interoperability isn’t just a local issue; it’s a global priority. A recent worldwide analysis found that a staggering 84% of healthcare organizations now consider interoperability essential to how they operate.
This widespread agreement is pushing major trends forward, like the rise of AI-embedded EHRs designed to handle enormous amounts of data, look at the UK’s NHS, which manages 1.6 million interactions every day. Health systems across the globe are racing to upgrade their infrastructure to support better data sharing and AI integration. You can discover more insights about 2026 health IT predictions to see where things are headed.
This global momentum signals a fundamental shift in thinking. Connected healthcare is no longer an optional upgrade; it’s the mandatory foundation for safe, efficient, and patient-first medicine.
Speaking the Same Language: Core Healthcare Data Standards
Imagine trying to build something complex, like a car, where every team uses a different set of measurements. The engine team uses inches, the chassis team uses centimeters, and the electronics team uses… well, something else entirely. It would be a disaster. That’s exactly what healthcare looks like without common data standards.
For different medical systems to actually talk to each other, they need a shared language—a set of rules and formats that everyone agrees on. These standards are the foundation of healthcare data interoperability services, ensuring that a lab result from one system means the exact same thing to a completely different system across town.
This is how we move from a collection of disconnected data points to a complete, coherent story for every patient.
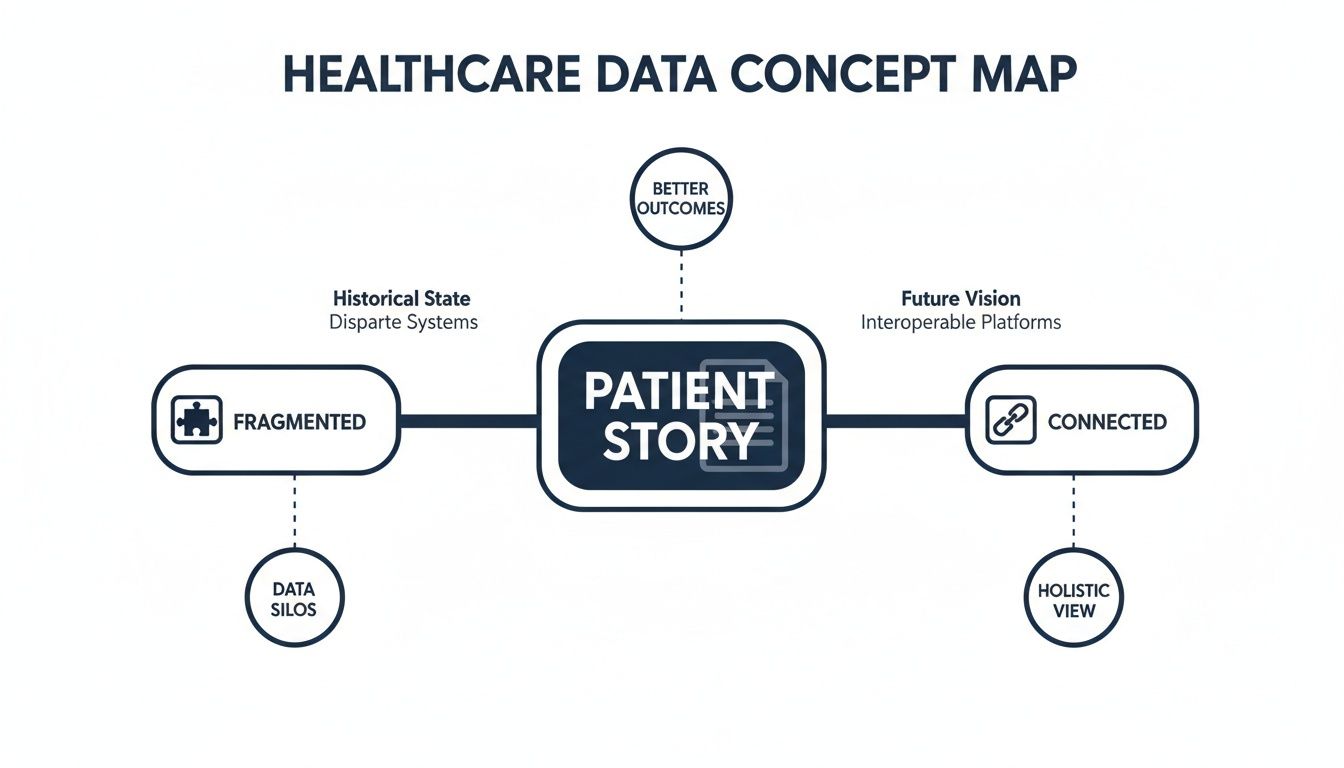
The journey from fragmented records to a unified patient view is only possible when all systems are speaking the same technical language. Let’s break down the most important ones.
The Old Guard and the New Wave: HL7, IHE, and FHIR
For a long time, the dominant language was Health Level Seven (HL7). Specifically, versions like HL7v2 were the workhorses of the industry, creating a message-based system for sending things like patient admissions, orders, and results between hospital systems. It got the job done, but it was a product of its time—often rigid, complex, and a real headache to integrate with modern web or mobile apps.
To solve more complex workflow problems, Integrating the Healthcare Enterprise (IHE) came along. IHE doesn’t create new standards but provides implementation guides, or “profiles,” showing how to use existing standards like HL7 and DICOM (for imaging) to address specific clinical needs, like managing radiology workflows or sharing patient documents.
Then came the game-changer: Fast Healthcare Interoperability Resources (FHIR).
FHIR (pronounced “fire”) isn’t just an update; it’s a complete rethink. It was built from the ground up using the same modern web technologies that power the apps we use every day, making health data far more accessible, flexible, and developer-friendly.
FHIR’s rise is a direct response to the needs of today’s connected health ecosystem. It’s what makes modern healthcare software development projects possible, enabling everything from patient-facing apps to sophisticated analytics platforms.
So, why is everyone so excited about FHIR?
- It Thinks Like the Web: FHIR uses RESTful APIs, the same technology behind your favorite social media or banking app. This makes it incredibly straightforward for developers to build applications that can securely pull and push health data in real-time.
- It Uses “Resources” as Building Blocks: Instead of clunky, all-or-nothing messages, FHIR breaks data into small, logical chunks called “Resources”—like a Patient, an Observation, or a Medication. These can be mixed and matched as needed, offering incredible flexibility.
- It’s Easy to Read: Data is formatted in JSON or XML, which developers love because they are easy for both humans and computers to understand. This drastically speeds up development, testing, and troubleshooting.
Comparing Key Healthcare Interoperability Standards
Choosing the right standard depends entirely on the job you need to do. A hospital sending admission notices has different needs than a startup building a patient-facing mobile app. This table breaks down the key players to help you see where each one shines.
| Standard | Primary Use Case | Data Format | Key Advantage |
|---|---|---|---|
| HL7 v2 | Traditional in-hospital messaging (admissions, orders, results) | Pipe-and-hat (delimited text) | Widespread legacy adoption; deeply embedded in existing systems. |
| IHE | Standardizing complex clinical workflows (e.g., radiology) | Varies (uses other standards) | Provides a “recipe book” for solving real-world integration challenges. |
| FHIR | Modern web/mobile apps, real-time data access, APIs | JSON, XML | API-first, developer-friendly, and highly flexible for modern use cases. |
While older standards like HL7v2 remain essential for legacy systems, FHIR is clearly the future. It’s the engine driving the next generation of connected health applications and services.
This momentum is reflected in the market itself. The global healthcare interoperability solutions market hit USD 3.42 billion in 2023 and continues to climb, largely thanks to the new possibilities unlocked by standards like FHIR. As government mandates and patient expectations push for more open data, you can read the full research about this market growth to grasp just how quickly this space is evolving. Making a smart, forward-looking choice on standards is no longer just a technical decision—it’s a core business strategy.
Choosing the Right Architecture for Data Integration
Building a connected healthcare ecosystem is a lot like designing a city’s infrastructure. It’s not enough to just pave a few roads. You need a master plan, a network of highways, local streets, and smart traffic systems to keep everything moving. The architectural model you pick for your healthcare data interoperability services is that master plan. It dictates how data moves, how systems talk to each other, and whether your setup can handle what’s coming next.
Getting this blueprint right is more than just an IT decision; it’s a strategic one. It will determine if your organization can embrace new technologies, scale up telehealth, or get ready for AI-driven medicine. The right architecture ensures data doesn’t just flow, it flows intelligently.
Models for Connecting Your Digital Ecosystem
Think of each of your healthcare systems, the EHR, the lab system, the billing platform, as a distinct neighborhood in your city. To connect them, you have a few “urban planning” strategies to choose from, each with its own trade-offs.
- Point-to-Point Connections: This is the most basic approach. It’s like building a direct road between every single house that needs to communicate with another. It works when you only have a few houses, but as your city grows, you end up with a chaotic, unmanageable spaghetti junction of roads.
- Hub-and-Spoke Model: A more organized plan. Here, you place a central integration engine or data warehouse at the city’s center, and all traffic has to pass through it. This standardizes the flow and simplifies connections, but it also creates a major bottleneck and a single point of failure. If the central hub goes down, the entire city grinds to a halt.
- Microservices Architecture: This is the modern, decentralized city plan. Instead of one giant, monolithic system, you break down functions into small, independent services (the microservices) that communicate through lightweight APIs. It’s a flexible, resilient, and incredibly scalable network where you can add new neighborhoods or upgrade old ones without shutting down the whole city.
This choice is a cornerstone of any effective healthcare software development initiative, setting the stage for all future growth and innovation.
APIs as Bridges and ETL as Freight Lines
To really understand these models, it helps to think about the two main ways data gets from point A to point B.
APIs (Application Programming Interfaces) are like nimble, on-demand bridges connecting different parts of your city. They enable real-time, two-way communication, which is perfect for when a doctor needs to instantly pull a patient’s latest lab results from one system directly into another. They are built for the fast-paced, moment-to-moment needs of clinical care.
ETL (Extract, Transform, Load) processes, on the other hand, are the city’s heavy-duty freight train system. They’re designed to move massive volumes of data in bulk, usually on a set schedule. Think of this as the overnight train that hauls an entire hospital’s daily billing records over to the central finance system. It’s reliable and perfect for huge data migrations, but it’s not meant for real-time requests.
A truly robust architecture will almost always use both. A smart integration strategy depends on a partner skilled in custom software development who knows how to blend the immediacy of APIs with the sheer power of ETL. This balanced approach creates a data infrastructure that is both responsive and ready for large-scale analytics. To dive deeper into the nuts and bolts of building these systems, as we explored in our guide, digital health platform engineering is a great resource.
Ultimately, picking an architecture isn’t just a technical task. It’s a foundational business decision that directly impacts your scalability, costs, and ability to innovate. By choosing a model that aligns with your long-term vision, you’re not just solving today’s data-sharing problems—you’re building for the future of connected care.
How AI Supercharges Healthcare Interoperability
Getting healthcare data to move between systems is one thing. Making sure it’s understood, in context, is another challenge entirely. This is where Artificial Intelligence (AI) and Machine Learning (ML) come into play, turning a simple data pipeline into a source of powerful, actionable intelligence.
Think of AI as an expert translator and interpreter working tirelessly behind the scenes. It doesn’t just pass along a message; it understands its meaning, standardizes the language, and adds crucial context. This is the key to solving the semantic interoperability puzzle, ensuring the meaning of the data isn’t lost in translation from one system to the next.
From Connected Data to Intelligent Insights
AI algorithms are brilliant at spotting the subtle patterns, anomalies, and connections buried in massive clinical datasets—things a human analyst might easily miss. They add a sophisticated analytical layer on top of your connected data network, transforming it from a passive repository into a proactive, intelligent healthcare engine.
The industry is already moving fast in this direction. A 2026 global survey of over 21,500 healthcare software buyers found that FHIR/API interoperability was a top-three requirement for 92% of respondents. It’s become the price of entry.
Even more telling, the same survey found that markets adopting interoperability faster also showed 12 percentage points higher AI production deployment rates. The link is clear: seamless data exchange is the foundation for successful AI. You can learn more about these global healthcare IT survey findings to see the full picture.
This trend underscores a critical reality for healthcare leaders: a rock-solid interoperability strategy is the launchpad for any meaningful AI initiative.
Practical Use Cases for AI-Enhanced Interoperability
When you combine AI with truly interoperable data, you unlock capabilities that can fundamentally change clinical workflows and patient outcomes. It’s about much more than just cleaning up data fields.
- AI-Powered Clinical Decision Support: Picture an AI constantly monitoring a patient’s incoming data—EHR updates, lab results from an outside clinic, and pharmacy records. It can spot a potential drug interaction or flag the early signs of sepsis, alerting clinicians in real-time long before a crisis hits.
- Generative AI for Clinical Summaries: Clinicians are drowning in data. Generative AI can comb through decades of unstructured notes and reports from multiple systems and, in seconds, produce a concise summary of a patient’s entire history, highlighting what matters most.
- Predictive Analytics for Population Health: By analyzing aggregated, de-identified data from across a health network, AI models can forecast disease outbreaks, pinpoint at-risk populations, and help public health officials deploy resources where they’ll have the greatest impact.
Overcoming the Semantic Gap
One of the oldest and most stubborn problems in healthcare IT is the “semantic gap”—different systems using different terms for the same concept, like “heart attack” versus “myocardial infarction.”
AI, and especially Natural Language Processing (NLP), is the perfect tool to bridge this gap. It can understand the context behind the words, mapping dozens of different medical terms to a single, standard concept. This ensures that when data is shared, its clinical meaning stays perfectly intact.
By automatically cleansing, normalizing, and contextualizing data from countless sources, AI makes interoperable data not just available but truly useful at the point of care. For a deeper look into this area, as we explored in our guide, you can check out our guide on the future of AI in healthcare.
Ultimately, AI is the engine that transforms the promise of connected data into the reality of smarter, safer, and more efficient healthcare.
Navigating Security and Compliance in Data Sharing
In healthcare, you can’t talk about sharing data without talking about protecting it. They’re two sides of the same coin. While seamless healthcare data interoperability services are the goal, that goal is meaningless if it isn’t built on a rock-solid foundation of security and patient trust. Moving data isn’t the hard part; moving it safely is.
This means security can’t be an afterthought. It has to be woven into the very fabric of your data architecture from day one. For any organization touching patient information, compliance isn’t just a box to check—it’s a fundamental part of staying in business.

Core Pillars of a Secure Interoperability Framework
So, how do you build a system that’s secure by design? It comes down to a few critical components working in concert. These are the practical strategies that turn dense regulatory text into real-world protection for a patient’s most sensitive information.
- End-to-End Encryption: Think of this as a digital armored car. Data must be scrambled and unreadable both while it’s moving between systems (in transit) and while it’s sitting in a database (at rest). If someone manages to intercept it, all they get is gibberish.
- Role-Based Access Controls (RBAC): A receptionist doesn’t need to see a patient’s full surgical history. RBAC enforces the principle of least privilege, ensuring people can only see and touch the specific data they absolutely need to do their jobs. This dramatically cuts down on the risk of internal breaches, accidental or otherwise.
- Comprehensive Audit Trails: Every single time someone views, edits, or shares patient data, it needs to be logged. These detailed audit trails are non-negotiable for accountability and are your first line of defense when investigating a potential security incident.
- Robust Consent Management: Patients own their data. A modern interoperability solution must give them clear, transparent control over how that data is used and shared, honoring their preferences at every turn.
A truly secure interoperability ecosystem works on a ‘zero-trust’ model. The core idea? Trust no one by default. Every single request to access data must be verified, every time, whether it’s coming from inside or outside your network. It’s a powerful shift in mindset that guards against modern, sophisticated threats.
Adhering to Global Regulatory Standards
The web of healthcare regulations is notoriously complex. In the United States, we have HIPAA. In Europe, it’s GDPR. Both come with iron-clad requirements for protecting patient data.
Getting this wrong isn’t an option. The penalties for violations are steep, and the damage to your reputation can be impossible to repair. This is why any partner you choose for healthcare data interoperability services must have proven, deep expertise in building compliant solutions. It’s not enough to know the rules; they have to know how to translate them into technical safeguards and airtight operational policies. This practical guide to secure document sharing is a great resource that breaks down the essential legal and technical guardrails.
Building software that lives up to these standards is a highly specialized skill. As we cover in our guide to HIPAA-compliant software development, every architectural decision and line of code must be viewed through the lens of security and privacy. This proactive approach ensures your interoperability project doesn’t just connect systems. It protects the very people those systems are meant to serve.
A Practical Roadmap for Your Interoperability Project
Kicking off a healthcare data interoperability project can feel a lot like planning a major city-wide infrastructure overhaul. It’s a huge undertaking that demands a clear vision, a step-by-step plan, and the right team to pull it off. Without a solid roadmap, you risk ending up with a collection of disconnected efforts instead of a truly connected care experience.
The first move is always to take a hard look at your current tech stack. This isn’t just about making a list of software; it’s about digging in to find exactly where critical data gets stuck. Pinpointing these silos—whether they’re in billing, clinical workflows, or patient portals—is the only way to design a solution that solves actual business problems.
Phase 1: Laying the Foundation
Once you have a map of your current mess, you need to define what “done” looks like. What’s the end game? Maybe success is cutting redundant lab tests by 15%. Or perhaps it’s slashing patient intake times in half. These specific, tangible goals will become the North Star for your entire strategy.
With your objectives set, the next priority is building a strong data governance framework. This isn’t just about writing rules; it’s about creating clarity and accountability. A good governance plan will:
- Define data ownership: Make it crystal clear who is responsible for the quality and security of each data set.
- Establish data quality standards: Set the ground rules for how data is entered, formatted, and checked across every system.
- Outline stakeholder roles: Spell out who gets to manage, access, and secure patient information.
Getting this foundation right ensures that when you start connecting systems, the data flowing between them is actually reliable, secure, and trustworthy.
Phase 2: Execution and Measurement
Choosing the right technology partner is a make-or-break decision. You need someone with a proven track record not just in integration, but specifically in healthcare data interoperability services. They have to know standards like FHIR inside and out and have a portfolio of successful projects to back it up. As our own client cases show, a partner’s ability to execute a phased, strategic implementation is what separates success from failure.
A successful interoperability project is never a “big bang” launch. It’s a series of well-planned phases, each delivering incremental value and building momentum for the next stage. This iterative approach minimizes risk and allows for continuous improvement.
Finally, you have to measure what matters. Define your Key Performance Indicators (KPIs) from day one so you can track progress against those initial goals. Don’t just focus on technical milestones; measure the real-world business impact.
- Reduced Administrative Costs: How much time and money are you saving by automating tasks that used to be manual?
- Improved Care Coordination: Are you seeing fewer repeated tests? Are referral times getting shorter?
- Enhanced Clinician Satisfaction: Ask your clinicians. Is it easier for them to get a complete picture of a patient’s health?
This kind of roadmap turns a daunting technical challenge into a manageable, strategic initiative. By focusing on a phased approach, strong governance, and clear metrics, you can build a connected healthcare system that delivers lasting value to your organization and, most importantly, to the patients you serve.
Frequently Asked Questions About Healthcare Data Interoperability Services
What is the difference between interoperability and integration?
It’s easy to confuse these two, but the distinction is crucial. Integration is about building the pipes—it’s the technical work of getting data to move from one system to another. Think of it as connecting System A to System B. Interoperability, on the other hand, is about what happens when the data arrives. It’s about ensuring that System B can actually understand and use the information from System A without a human needing to translate it. This is the real end goal for any serious healthcare software development initiative.
How does FHIR improve on older standards like HL7 v2?
Simply put, FHIR was designed for the internet age. Older standards like HL7 v2 were groundbreaking in their day, but they rely on rigid, cumbersome messaging formats. FHIR uses modern, web-based RESTful APIs and breaks down complex health information into small, logical “Resources.” This modular approach makes data exchange incredibly fast and flexible, which is why FHIR is the backbone for so many modern mobile health apps and cloud-based platforms. It’s a game-changer for any AI solutions partner looking to innovate quickly.
What are the biggest barriers to achieving interoperability?
The technical challenges are real, but they often aren’t the biggest hurdles. The roadblocks that truly stall progress are usually a mix of financial, organizational, and cultural issues. We consistently see organizations grapple with the cost of modernizing legacy systems, gaps in data standardization, complex governance and politics, and concerns over security and privacy. Getting past these requires a solid strategic plan and a partnership with a custom software development team that knows how to navigate these complexities.
How can we measure the ROI of an interoperability project?
Measuring the return on investment for interoperability goes beyond just hard numbers. Quantitatively, you can track concrete financial gains like a reduction in duplicate tests, lower administrative costs, and accelerated revenue cycles. Qualitatively, the impact is just as important. Measure improvements in clinician satisfaction, patient safety due to fewer medical errors, and ultimately, better health outcomes. A true ROI calculation also has to factor in the long-term strategic value of being able to innovate faster and stay competitive.
Ready to unlock the full potential of your healthcare data? At Bridge Global, we specialize in building secure, scalable, and intelligent interoperability solutions. Discover the power of AI for your business and start your journey toward a truly connected care ecosystem today. Get in touch with our experts today.



