A Guide to Healthcare Cloud Transformation
At its core, healthcare cloud transformation is the process of moving a healthcare organization’s digital backbone: its data, applications, and core IT systems, from physical, on-site servers to the cloud. But this is far more than just a technical switch. It’s a fundamental rethinking of how to build a more agile, secure, and patient-centric healthcare ecosystem that can actually keep up with modern medicine and patient demands.
Why Cloud Transformation Is No Longer Optional in Healthcare
For decades, healthcare IT was defined by sprawling, on-premise data centers. These were expensive to build, costly to maintain, and notoriously slow to adapt. In today’s world, that old model is buckling under the pressure from relentless medical innovation, the explosion of health data, and patients who expect digital-first experiences.
This is why healthcare cloud transformation has shifted from a “nice-to-have” IT project to a core strategic necessity. It’s the new foundation for the future of care.
The table below breaks down the primary motivations pushing organizations to the cloud and the powerful advantages they gain by doing so.
Core Drivers and Strategic Benefits of Adopting the Cloud
| Key Driver | Strategic Advantage |
|---|---|
| Skyrocketing Infrastructure Costs | Converts unpredictable capital expenses into manageable operating costs. |
| The Data Explosion | Provides nearly infinite scalability to handle massive data from EHRs, imaging, and genomics. |
| Rising Patient Expectations | Enables the rapid development of digital services like telehealth and patient portals. |
| Need for Interoperability | Breaks down data silos, allowing for a unified view of patient and operational data. |
| Security & Compliance Demands | Offers advanced, specialized security tools and simplifies regulatory adherence. |
| Innovation & Analytics | Unlocks the ability to integrate AI and machine learning for predictive insights. |
These drivers and benefits aren’t just theoretical; they represent a clear path away from the limitations of the past and toward a more intelligent, responsive model of healthcare.
The real game-changer here is how the cloud dismantles data silos. For years, critical information was trapped in separate systems across different departments.
The true power of the cloud in healthcare is its ability to create a single source of truth. When clinical, financial, and operational data can be securely accessed and analyzed together, it unlocks insights that directly improve patient outcomes and fix broken workflows.
As an experienced AI solutions partner, we’ve seen this firsthand. This shift truly modernizes healthcare from the ground up.
By moving to the cloud, organizations lay the essential groundwork for advanced healthcare software development. It opens the door to powerful analytics and AI, turning mountains of raw data into life-saving clinical intelligence. This transition isn’t just about where your data lives; it’s about what you can finally do with it.
Navigating Security and Compliance in the Cloud
For any healthcare leader I talk to, the conversation about moving to the cloud always comes back to one thing: security. It’s the multi-billion dollar question. How can we possibly move sensitive Protected Health Information (ePHI) into the cloud and still sleep at night, knowing it’s secure and compliant?
There’s a common and understandable fear that the cloud is somehow less secure than a server locked in a room down the hall. In reality, the security infrastructure built by major cloud providers is more robust than what most healthcare organizations could ever build or afford on their own.
But here’s the critical piece of the puzzle: cloud security isn’t something you just buy; it’s a partnership you actively manage. This is where the Shared Responsibility Model comes into play.
Think of it like this: your cloud provider, whether it’s Amazon Web Services, Microsoft Azure, or Google Cloud, is like the landlord of a high-tech, ultra-secure office building. They’re responsible for the physical security of the building: the reinforced walls, the security guards at the door, the surveillance systems, the resilient power grid. In tech terms, this is security of the cloud: the physical data centers, the servers, the core network.
You, as the tenant, are responsible for what happens inside your office. You decide who gets a keycard (access management), what files you leave on the desks (your data), and whether you lock your filing cabinets (encryption). This is security in the cloud. It’s on you to configure your applications, manage user credentials, and protect the data you place there.
Meeting Key Regulatory Mandates
Getting this partnership right is absolutely essential for meeting healthcare’s incredibly strict regulations. The big three you’ll be dealing with are HIPAA, HITRUST, and GDPR.
-
HIPAA (Health Insurance Portability and Accountability Act): This is the foundational U.S. law for protecting patient data. Any cloud service you use for ePHI must be HIPAA-compliant, and that starts with signing a Business Associate Agreement (BAA) with your provider. A BAA is a legally binding contract confirming that the provider will implement the necessary safeguards to protect patient information.
-
HITRUST (Health Information Trust Alliance): Think of HITRUST as a framework that builds on top of HIPAA and other standards, creating a certifiable security program. Achieving HITRUST certification is the gold standard, signaling to partners and payers that you have a mature and comprehensive security posture.
-
GDPR (General Data Protection Regulation): If you treat patients from the European Union, you can’t ignore GDPR. It’s a sweeping set of rules governing data privacy for all EU citizens, and the penalties for non-compliance are severe.
Essential Safeguards for Healthcare Data
Building a secure and compliant cloud environment isn’t about flipping a switch; it requires putting specific technical and procedural safeguards in place from day one. These aren’t optional; they’re the bedrock of a trustworthy system.
When you get security right in the cloud, it does more than just stop breaches; it builds patient trust. Showing a real commitment to data privacy with strong technical controls turns compliance from a headache into a competitive advantage.
Here are the non-negotiables we build into every project:
-
End-to-End Encryption: All data must be encrypted, period. This applies whether it’s “at rest” sitting in a database or “in transit” moving across the network. Encryption means that even if someone manages to intercept your data, it’s just unreadable gibberish without the right keys.
-
Identity and Access Management (IAM): IAM policies are your digital gatekeepers. They enforce the principle of least privilege, which is a fancy way of saying people should only have access to the exact information they need to do their job, and nothing more. A clinician doesn’t need access to billing systems, and an administrator doesn’t need to see patient charts.
-
Continuous Monitoring and Logging: One of the most powerful features of the cloud is the ability to see everything that’s happening in your environment in real-time. We set up automated monitoring and alerts to flag any suspicious behavior instantly, allowing security teams to jump on a potential threat before it can cause any damage. As we explored in our guide, establishing strong governance in the cloud is essential for maintaining this level of control.
Choosing the Right Cloud Architecture for Healthcare
Picking a cloud architecture for your healthcare organization isn’t just a technical decision; it’s like drawing up the blueprint for a new hospital. The foundation you lay today will directly impact your team’s efficiency, the security of patient data, and your ability to innovate for years to come. A poor choice here can lead to expensive fixes and serious security gaps down the road.
The first step is to get a handle on the basic service models. These aren’t just acronyms; they define how much of the technical heavy lifting you do versus what the cloud provider handles for you.
Understanding the Core Cloud Service Models
Each model strikes a different balance between control and convenience. The right one for you depends entirely on your team’s technical skills, your budget, and what you’re trying to accomplish.
-
Infrastructure as a Service (IaaS): Think of IaaS as leasing a brand-new, empty hospital building. You get the fundamental infrastructure: the secure space, the power, the plumbing (servers, storage, networking), but it’s up to you to bring in everything else. You’re responsible for the operating systems (the operating tables) and all the applications (the MRI machines). This model gives you maximum control, which is great for organizations with unique IT requirements and the expert staff to manage it all.
-
Platform as a Service (PaaS): PaaS is more like leasing a fully-equipped operating room. The core infrastructure and development tools, like databases, analytics software, and operating systems, are already set up and maintained for you. This lets your team focus purely on their primary job: building and running your unique healthcare applications, without getting bogged down in managing the underlying hardware and software.
-
Software as a Service (SaaS): This is the most hands-off approach, similar to subscribing to a specialized telehealth service. You don’t own the platform or manage any of the tech behind it. You simply pay a fee to use a finished application, like an Electronic Health Record (EHR) or a medical billing system. It’s the simplest option and offers the fastest path to getting a new capability online.
As you build out your cloud environment, it’s worth looking into managed database solutions like an RDS Relational Database Service to simplify data management, no matter which service model you lean on.
The Rise of the Hybrid Cloud in Healthcare
While each model has its place, the complex reality of healthcare rarely fits into a single box. This is precisely why the hybrid cloud model has become the go-to strategy for so many providers. It smartly blends the control and security of a private cloud (your own on-premise servers) with the flexibility and power of a public cloud.
It’s like having a secure, on-site vault for your most sensitive patient data while using a world-class, off-site research lab for big data analytics and new application development. You get the best of both worlds.
The hybrid cloud isn’t a compromise; it’s a strategic choice. It allows healthcare organizations to modernize and innovate with public cloud services while keeping a firm grip on the security and compliance of their most critical data assets.
This isn’t just a niche trend; the market data backs it up. The healthcare cloud market is shifting decisively toward hybrid models, which are expected to have the highest growth rate. This architecture is a direct answer to compliance headaches, letting providers keep protected health information on private, controlled infrastructure while shifting other workloads to more cost-effective public clouds.
Europe provides a great real-world example of this model’s success. Today, about 68% of hospitals there use cloud-based patient records, often within a hybrid framework to balance innovation with regulation. You can dive deeper into these architectural trends and market projections.
Ultimately, your architectural choice is a cornerstone of your healthcare cloud transformation. It demands a clear-eyed assessment of your clinical workflows, data governance rules, and future goals. Working with partners who truly understand the fine points of healthcare software development will ensure your blueprint is built not just for today’s needs, but for the challenges of tomorrow.
Unlocking Advanced Analytics and AI with the Cloud
Moving to the cloud is about more than just swapping out old servers for new ones; it’s about finally unlocking the incredible potential hidden inside your organization’s data. The cloud provides the raw horsepower needed for advanced analytics and artificial intelligence – technologies that are completely reshaping how healthcare is delivered. Without its massive scale, these data-hungry tools would simply be too expensive and complex for most organizations to even consider.
Think of your old on-premise servers like a small-town library. It’s useful, for sure, but its shelves and reading rooms are limited. The cloud, on the other hand, is like the entire global internet of information – a near-infinite resource that can process staggering amounts of data from EHRs, medical imaging, and wearable IoT devices all at once. That’s a job that would bring any traditional system to its knees.
From Reactive Care to Predictive Insights
The real magic happens when you stop just storing data and start using it to see what’s coming next. Cloud-based AI and machine learning models can dig through petabytes of patient information to spot patterns that are impossible for humans to see. This is how you make the critical shift from reacting to problems to proactively preventing them.
This isn’t just theory. Here’s how it’s making a difference today:
-
Predictive Analytics for At-Risk Patients: AI algorithms can analyze patient histories and real-time data streams to flag individuals at high risk for conditions like sepsis, heart failure, or readmission. This gives care teams a crucial heads-up, allowing them to step in before a crisis hits.
-
AI-Enhanced Diagnostic Imaging: Machine learning, trained on millions of past scans, can help radiologists by highlighting subtle anomalies in X-rays, CTs, and MRIs. The result is a faster, more accurate diagnosis.
-
Personalized Treatment Plans: By crunching genomic data, lifestyle details, and treatment results from thousands of similar cases, AI helps clinicians tailor care plans that have a much better chance of success for each unique patient.
This isn’t science fiction. AI is already empowering healthcare providers to turn their data from a simple record of what has happened into a powerful tool that predicts what will happen. That shift directly translates to better patient outcomes.
The momentum is undeniable. A full 73% of healthcare providers are already using cloud-based AI for diagnostics and predictive analytics. In fact, the AI in healthcare market is expected to rocket past $45 billion by 2026, and cloud platforms are driving the charge, making up over 60% of these implementations. A recent report on the global healthcare cloud market confirms this trend. The cloud makes it possible to deploy these powerful models without the crushing upfront cost of buying and maintaining the necessary hardware.
Building Your AI Capabilities on a Solid Foundation
Tapping into this power requires a smart plan. It all starts with creating a solid, secure cloud data warehouse to bring all your information together from its various silos. Once your data is in one place, you can start layering on advanced analytical tools and custom machine learning models. As we explored in our guide, a well-planned healthcare analytics implementation is the bridge between raw data and genuine clinical intelligence.
This is often where bringing in an experienced technology partner makes all the difference. Our expert AI development services are built to guide healthcare organizations through this exact process. We help you design and deploy custom AI solutions that tackle your specific challenges, whether that’s streamlining hospital operations or boosting diagnostic accuracy.
Using AI for your business is no longer a “nice-to-have”; it’s a core piece of any modern healthcare strategy. By making the move to the cloud, you aren’t just getting an IT upgrade. You’re laying the foundation for a smarter, more predictive, and truly patient-focused future.
Your Phased Roadmap to a Successful Cloud Migration
Trying to move a healthcare organization to the cloud without a detailed roadmap is like performing surgery without a pre-op checklist. It’s a recipe for chaos, risk, and almost certain failure. A successful journey requires a deliberate, phased approach, one that goes far beyond a simple “lift-and-shift”, to ensure patient care never misses a beat while you unlock long-term benefits.
Breaking the project into manageable stages is the key to de-risking the entire process and building momentum. This strategic roadmap will guide your organization from the initial assessment all the way to ongoing innovation, making sure every step adds real value and aligns with your clinical and operational goals.
This visual flow breaks down the four essential phases of a structured healthcare cloud migration, from initial discovery to continuous improvement.
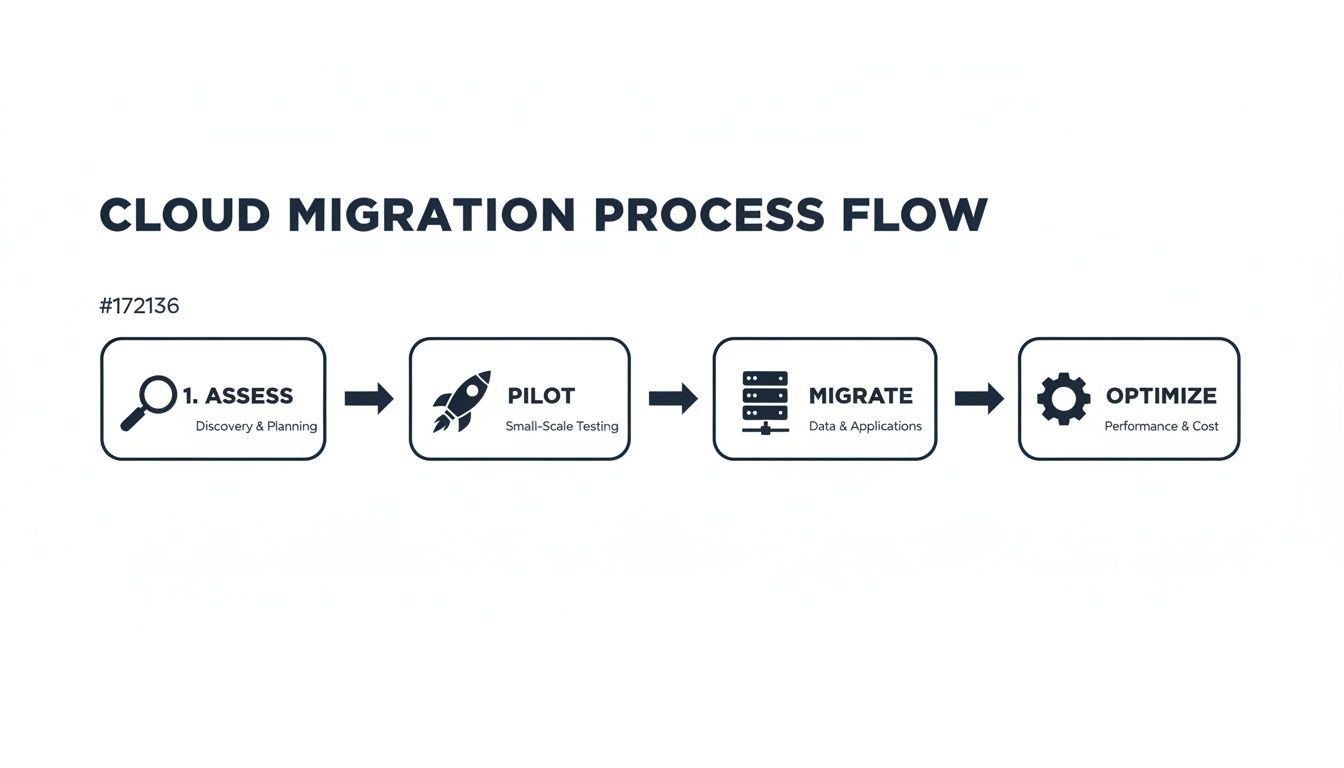
Following this process ensures that each stage builds on the last, creating a solid foundation for a scalable, secure, and compliant cloud environment.
Phase 1: Assessment and Planning
This is where you draw the blueprint for the entire project. Rushing this stage is a classic mistake, one that almost always leads to budget blowouts and mountains of technical debt down the road. The goal here is to get an almost painfully deep understanding of your current IT environment and define exactly what success will look like.
Key activities in this phase include:
-
Application Portfolio Analysis: You need to map out every single application, from your core EHR and PACS systems to the small departmental billing software nobody’s touched in years. This means classifying each one based on its complexity, how critical it is to operations, and its readiness for the cloud.
-
Dependency Mapping: This is about uncovering the intricate web of connections between applications, databases, and infrastructure. Skipping this step is how you get unexpected outages when you start moving what you thought was a standalone system.
-
Defining Success Metrics: Establish clear, measurable Key Performance Indicators (KPIs). These need to go beyond just cost savings. Think about clinical metrics like reducing EHR latency for physicians or improving how quickly care teams can access patient data.
Phase 2: Pilot and Foundation
With a solid plan in hand, it’s time to build your cloud “landing zone” and test the waters with a pilot project. This is absolutely not the time to move your most complex, mission-critical system. Instead, pick a low-risk but high-impact workload to validate your strategy and build some confidence across the organization.
The pilot phase accomplishes several crucial things. It gives your team hands-on experience in the new cloud environment, lets you test security controls and compliance protocols in a real-world setting, and, importantly, delivers some early wins to show stakeholders. A successful pilot proves your strategy is sound and paves the way for wider adoption.
A well-chosen pilot project is your proof-of-concept for the entire migration. It validates technical assumptions, helps you refine migration processes, and builds the organizational buy-in you’ll need to tackle the bigger, more complex workloads later.
Phase 3: Phased Migration
Now the real work begins. Instead of a “big bang” approach where you try to move everything at once (don’t do that), you migrate applications in strategic waves. This iterative process dramatically minimizes disruption and lets your team learn and adjust as you go.
You can group applications based on different criteria: by clinical department, business function, or even technical architecture. For instance, you might start with administrative and HR systems, then move to ancillary clinical applications, before finally tackling the core EHR and medical imaging archives. This methodical approach lets your team focus its resources effectively and manage the complexity of each wave. Our own experience with complex custom software development confirms that breaking big projects into manageable sprints is the only way to succeed.
Phase 4: Optimization and Innovation
Getting to the cloud isn’t the finish line; it’s the starting line for true innovation. Once your workloads are running in their new home, the focus shifts to continuous optimization. This means right-sizing resources to control costs, fine-tuning application performance, and constantly strengthening your security posture.
This is also where your organization can finally tap into powerful cloud-native services. You can start integrating advanced analytics, exploring machine learning for predictive care, and developing new digital experiences for patients. This final phase turns the cloud from just infrastructure into a real engine for growth and better patient outcomes, something we’ve seen firsthand in our successful client cases.
Calculating Your ROI and Choosing the Right Partner
Shifting your healthcare organization to the cloud is a massive undertaking, both strategically and financially. Getting the green light from stakeholders and setting yourself up for success means building a business case that goes way beyond just saving a few bucks on server costs. It’s all about a smarter way of thinking about Return on Investment (ROI) and being incredibly diligent when picking the right partner to get you there.
A realistic ROI calculation for a healthcare cloud transformation has to look past the hardware you’re unplugging. The real wins are in the clinical and operational improvements that directly boost patient care and strengthen your financial health.
Beyond Infrastructure Savings: The True Value of Cloud
To build a truly compelling financial case, you need to show the value across a few key areas:
-
Clinical Productivity: Think about the time saved per clinician, per day, just from faster EHR access and less system lag. Even saving a few minutes for each doctor or nurse adds up to thousands of reclaimed hours every year – time that goes right back to patient care.
-
Operational Efficiency: How much better can your back-office run? Cloud tools can automate tedious processes like billing and claims, which means fewer manual errors and a faster revenue cycle. That’s real money, fast.
-
Improved Patient Outcomes: This is where it gets powerful. Analyze how cloud-based analytics can help you lower patient readmission rates or spot at-risk groups earlier. Every single readmission you prevent is a huge cost saving and a massive win for patient well-being.
-
Reduced Security Risk: Don’t forget about cost avoidance. The investment you make in top-tier cloud security is a tiny fraction of the fines, legal fees, and reputational damage that come with a major data breach.
The most compelling ROI for cloud transformation isn’t found in a server room; it’s realized in the exam room. When technology frees clinicians to spend more time with patients and less time fighting with slow systems, everyone wins.
Selecting Your Cloud Transformation Partner
Picking the right partner is probably the single most important decision you’ll make. You’re not just looking for a vendor; you need a strategic guide who lives and breathes this stuff. As you vet your options, put a premium on firms with a deep history in healthcare, because a general IT shop simply won’t get the nuances of our industry.
Look for a partner who can clearly show you they have:
-
Proven Healthcare & Compliance Expertise: They need a rock-solid history of working in HIPAA and HITRUST environments and must be ready to sign a Business Associate Agreement (BAA) without hesitation.
-
A Collaborative and Transparent Approach: The best partners work with you, not just for you. They should be focused on transferring knowledge to your team so you’re not left in the dark after the project is done.
-
Future-Focused Technical Skills: They need to be experts in more than just moving data. Look for great skills in modern analytics and AI. This ensures the foundation you’re building today can support the innovations you’ll need tomorrow. As we explored in our guide, hiring a cloud strategy consultant offers additional valuable insights.
This journey requires a partner who gets both the technology and the mission of healthcare. Finding that right fit makes all the difference.
Frequently Asked Questions
Is the cloud really secure enough for patient data (ePHI)?
Yes, when implemented correctly. Major cloud providers like AWS, Azure, and Google Cloud invest billions in security, often exceeding the capabilities of on-premise data centers. The key is to follow the Shared Responsibility Model: the provider secures the cloud’s infrastructure, while your organization secures the data and applications within the cloud. This involves end-to-end encryption, strict access controls (IAM), and continuous monitoring. A signed Business Associate Agreement (BAA) with your provider is also a non-negotiable requirement for HIPAA compliance.
What is the biggest mistake to avoid in healthcare cloud transformation?
The most common mistake is performing a simple “lift-and-shift” migration without re-evaluating and optimizing workflows. This approach treats the cloud like a different data center, failing to leverage its true potential for agility, scalability, and innovation. A successful transformation requires collaboration between IT and clinical teams to redesign processes that capitalize on cloud-native capabilities, ensuring the technology directly supports better patient outcomes and operational efficiency.
How can we manage and control cloud costs effectively?
Controlling cloud costs requires a proactive strategy, often called FinOps (Cloud Financial Operations). Key practices include:
-
Right-sizing: Continuously analyzing usage and adjusting resources to match demand, avoiding over-provisioning.
-
Reserved Instances: Committing to long-term usage for predictable workloads to gain significant discounts.
-
Automation: Using scripts to shut down non-production environments (like development and testing) during off-hours.
-
Cost Allocation and Monitoring: Tagging all resources to specific projects or departments and setting up budget alerts to prevent unexpected spending.
Ready to start your transformation journey with a partner you can trust? Bridge Global offers expert guidance in cloud migration, security, and AI development services to ensure your success.



