Healthcare Digital Transformation: A Guide to Modern Care
Let’s get straight to it. When we talk about healthcare digital transformation, we’re not just talking about swapping paper charts for iPads. It’s a fundamental overhaul of how healthcare organizations operate and deliver care, all driven by technology.
The goal isn’t just to digitize the old way of doing things. It’s about creating entirely new, smarter pathways to manage patient health, improve outcomes, and make the whole system run more smoothly. This change is happening out of necessity: to bring down costs, boost the quality of care, and simply meet the expectations of today’s patients.
What Is Healthcare Digital Transformation, Really?
Forget the buzzwords for a moment. At its heart, healthcare digital transformation is about a complete rethink of care delivery. It’s like the jump from a paper road atlas to a live GPS app on your phone. You don’t just get a digital map; you get real-time traffic updates, alternate routes, and a much smarter way to get where you’re going.
This same evolution in healthcare is driven by an urgent need to shift from reactive sick-care to proactive, patient-focused well-care.

The global investment in this shift is massive, with spending expected to reach $4 trillion by 2027. This isn’t just money thrown at flashy tech; it’s a strategic response to some of the industry’s most persistent and costly problems.
The Core Goals Driving The Shift
Three main objectives really steer this transformation. Each one targets a major weak point in the traditional healthcare model, aiming to build a system that’s more resilient and in tune with patient needs.
Here’s what it’s all about:
-
Achieving Better Patient Outcomes: This means using data and tech for earlier diagnoses, crafting personalized treatment plans, and keeping an eye on patients remotely. The result? Genuinely better health.
-
Creating Smarter Operational Workflows: Think about automating all that mind-numbing administrative work, using resources more effectively, and making sure care teams can actually communicate. This helps cut down on staff burnout and operational waste.
-
Using Data to Make Informed Decisions: It’s about tapping into real-time data from all over the place to understand patient groups, see what treatments are working, and spot operational roadblocks before they become crises.
Digital transformation in healthcare is not just a technological upgrade. It represents a cultural shift toward a more integrated, data-driven, and patient-empowered model of care delivery.
From Paper to Predictive Analytics
Moving from stacks of paper files to an intelligent, connected digital system is a monumental task. It’s about so much more than just implementing electronic health records (EHRs). The real work is in building a connected ecosystem where data can flow securely and seamlessly between patients, providers, and payers.
This level of connectivity opens the door to incredible new capabilities, from monitoring a patient’s vitals at home to using AI to predict a potential health crisis before it happens.
2. The Core Technologies Powering Modern Healthcare
The big shift in healthcare isn’t happening because of a single invention. It’s powered by a set of interconnected technologies working in concert. Think of it like a high-performance engine; it’s not just one part, but a whole system of sensors, computers, and mechanical pieces that deliver a smooth, powerful ride. These digital tools are the engine driving change, reimagining everything from diagnostics to how care is delivered.
At the heart of it all is our newfound ability to gather, process, and act on massive amounts of health data, and to do it securely and intelligently. Each technology plays a specific part, whether it’s making a doctor accessible from anywhere or spotting health problems before they become emergencies.

To make sense of it all, here’s a quick breakdown of the main players and what they bring to the table.
Core Technologies in Healthcare Transformation
| Technology | Primary Function | Key Benefit |
|---|---|---|
| AI & Machine Learning | Analyzes complex data (images, records) to find patterns and make predictions. | Enables proactive care and personalized treatment plans. |
| Telehealth & RPM | Delivers virtual care and monitors patient vitals from a distance. | Breaks down geographic barriers, making care more accessible. |
| Cloud Computing | Provides a secure, scalable platform for storing and sharing health data. | Creates a connected ecosystem where data is available on demand. |
| Interoperability | Ensures different health IT systems can exchange and interpret data seamlessly. | Gives clinicians a complete, unified view of a patient’s health. |
Each of these is powerful on its own, but their real strength comes from how they work together to create a smarter, more connected healthcare system.
AI And Machine Learning: The Brains Of The Operation
Artificial Intelligence (AI) and Machine Learning (ML) are the analytical powerhouses making predictive and personalized medicine a reality. These systems are designed to sift through incredibly complex datasets: medical images, patient histories, genetic information, and spot patterns that even the most experienced doctor might miss. This is what helps shift healthcare from a reactive “fix it when it’s broken” model to a proactive one.
For example, an AI algorithm can look at a retinal scan and find the earliest signs of diabetic retinopathy, long before a patient even notices a change in their vision. In another case, an ML model can identify which patients are most likely to be readmitted to the hospital, giving care teams a chance to step in with extra support. As we explored in our guide on the role of AI in healthcare, these tools don’t replace clinicians; they give them data-driven superpowers.
Telehealth And Remote Patient Monitoring: Bridging The Distance
Distance has always been a major hurdle in getting good care, especially for people in rural areas or those who can’t easily travel. Telehealth and Remote Patient Monitoring (RPM) tackle this problem head-on by bringing the clinic into the patient’s home.
-
Telehealth platforms make virtual appointments possible, connecting patients with specialists no matter where they are. This has been a game-changer for routine check-ups, mental health support, and managing chronic conditions without the hassle of travel.
-
Remote Patient Monitoring (RPM) uses connected gadgets like smart blood pressure cuffs, glucose meters, or wearables to keep an eye on a patient’s vitals around the clock. This constant stream of data gives doctors a much clearer picture of a patient’s health between visits, so they can catch issues early.
The growth here is staggering. Digital health is booming, with global revenue projected to hit US$177.77 billion in 2026 and keep climbing. This explosion is driven by everyone having a smartphone, better internet access, and a global need to manage rising healthcare costs. Telehealth and mHealth apps are at the forefront, putting preventive care right in our hands. You can see these market trends for yourself on Statista.com.
Cloud Computing: The Secure And Scalable Foundation
None of this would work without a strong, secure, and flexible foundation to handle all the data. That’s where cloud computing comes in. It provides the digital backbone that lets healthcare organizations store, access, and share electronic health records (EHRs) and other sensitive information safely and efficiently.
By ditching bulky, on-site servers for the cloud, hospitals and clinics can cut infrastructure costs, tap into the top-tier security of specialized cloud providers, and make sure critical information is there for authorized staff whenever and wherever they need it.
This accessibility is what makes a truly connected healthcare system possible. When a specialist can instantly pull up a patient’s full medical history from a different hospital, or a wearable device can securely send data to a cloud platform for AI analysis, you start to see the real potential for better, faster care. This is exactly where expert AI development services are essential – building systems that are not only powerful but also compliant from the very start.
Why Digital Transformation Is a Smart Business Move
Improving patient care is the goal, but every healthcare leader has to ask: what’s the actual business case? What’s the tangible return on investment (ROI) when we take on something this massive? The answer is surprisingly clear. A strategic digital transformation isn’t just another IT expense; it’s a core business strategy that delivers real, measurable gains to your bottom line.
This is about moving technology from a background support role to the very heart of your growth and efficiency plans. When you weave digital tools into your daily operations, you start unlocking levels of performance you couldn’t reach before. In a market that’s changing faster than ever, this isn’t just an advantage; it’s a necessity.
Streamlining Operations Through Automation
One of the first places you’ll see a massive impact is in operational efficiency. We all know healthcare administration is bogged down by manual, repetitive tasks. They eat up time, drain resources, and are a breeding ground for human error. Digital automation is the perfect fix.
Imagine automating patient scheduling, billing, and insurance verifications. The result is a dramatic drop in administrative overhead, which directly impacts your budget. But more importantly, it frees up your highly skilled staff: nurses, doctors, and administrators, to focus on what they do best: high-value work that directly involves patients. This isn’t just a productivity boost; it’s a morale boost that helps reduce burnout.
Investing in smart healthcare software development allows you to build systems that handle these workflows automatically, leading to major cost savings and a much more agile organization.
By automating routine administrative tasks, healthcare organizations can reclaim up to 30% of their staff’s time, allowing them to focus on complex problem-solving and direct patient interaction.
Enhancing Patient Engagement and Loyalty
Let’s be honest, a great patient experience is no longer a “nice-to-have.” It’s a critical driver of business. Digital tools make the entire healthcare journey feel more connected, convenient, and personal, and that translates directly into patient loyalty and better outcomes.
Think about the ripple effects of:
-
Patient Portals: When patients have 24/7 access to their own health records, lab results, and care plans, they become active participants in their own health.
-
Telehealth Services: Offering virtual appointments is a game-changer for convenience. It cuts down on no-shows and makes healthcare accessible to people who might otherwise go without.
-
Personalized Communication: Simple automated reminders for appointments or medications, paired with educational content relevant to their condition, keep patients on track and engaged.
This creates a powerful, positive loop. Patients who feel connected and in control are more satisfied and more likely to stick to their treatment plans. This leads to better long-term health, which means fewer costly emergency visits and a loyal patient base that trusts you with their care.
Unlocking New Revenue Streams and Market Opportunities
Digital transformation is about more than just making your current operations better; it’s about opening doors to entirely new ways of generating revenue. Technology lets you expand your services far beyond the four walls of a clinic.
The sheer scale of this opportunity is staggering. The global AI in healthcare market is projected to skyrocket from $39 billion in 2025 to $504 billion by 2032. This explosive growth is driven by things like generative AI, which is poised to change everything from how we handle patient follow-ups to how we analyze risk. While many executives are still figuring out how to measure the ROI, the momentum is undeniable. You can get the full picture by exploring Deloitte’s 2026 global health care report.
What do these new revenue streams look like in the real world?
-
Subscription-based wellness programs that use data from wearables to offer personalized health coaching.
-
Remote Patient Monitoring (RPM) services for managing chronic diseases which are a billable service that also improves care.
-
Data analytics services that provide anonymized, high-level insights to pharmaceutical companies or research institutions.
By embracing these digital tools, healthcare organizations can innovate their business models, connect with new groups of patients, and build a more profitable and resilient future. As an experienced AI solutions partner, we’ve seen firsthand how these strategic moves pay off, turning providers into true market leaders.
Your Strategic Roadmap for Digital Implementation
Jumping into a healthcare digital transformation without a clear plan is like trying to build a hospital without blueprints. You might end up with something, but it won’t be efficient, scalable, or truly serve its purpose. A strategic roadmap is your blueprint. It’s much more than a simple timeline for new tech; it’s a complete framework that lines up your goals, resources, and people toward a single, unified vision. This ensures every dollar spent and every process changed directly leads to better outcomes.
This is where the rubber meets the road – where strategy becomes action. Your plan has to tackle your organization’s real, specific challenges, whether that’s frustrating patient wait times or tangled administrative workflows. A well-defined roadmap helps you sidestep expensive mistakes and guarantees that your investment in things like custom software development delivers real, lasting value. It’s all about being intentional and methodical.
Phase 1: Define Clear Goals and Success Metrics
Before you even think about technology, you have to define what winning looks like. This first step is all about honest self-assessment. What are the biggest headaches for your patients and staff right now? Don’t try to boil the ocean. Zero in on the high-impact areas where a digital fix can make the biggest, most noticeable difference.
Your goals need to be SMART – Specific, Measurable, Achievable, Relevant, and Time-bound.
-
Instead of: “We want to improve patient satisfaction.”
-
Try: “We will reduce patient wait times for specialist appointments by 20% within six months by implementing a new online scheduling system.”
That kind of clarity gives you a solid benchmark to measure against, making it easy to prove a tangible return on investment down the line. To get deeper into crafting this foundational plan, check out our guide on what makes a successful digital transformation strategy.
Phase 2: Select the Right Technology and Partners
With clear goals in hand, you can start looking for the right tools and, just as importantly, the right team. This isn’t about chasing the shiniest new object. It’s about finding solutions that actually fit; solutions that integrate smoothly with your current systems, are fully compliant with regulations like HIPAA, and can scale as your organization grows.
Choosing a partner is just as critical as choosing the tech. You need a team that gets the unique complexities of healthcare software development, not just a generic IT vendor. Look for a partner with a proven track record in the healthcare industry, someone who can be a strategic advisor, not just a line of code. A great AI solutions partner will dig deep to understand your specific needs and recommend a tech stack that’s perfectly aligned with your goals.
A successful digital partnership is built on shared understanding. The right partner doesn’t just build what you ask for; they help you discover what you truly need to solve your core business challenges.
Phase 3: Implement Through Pilot Programs
Going “all-in” with a massive, organization-wide rollout from day one is a recipe for chaos. A much smarter approach is to start small with focused pilot programs. Pick a single department, a specific clinic, or one workflow to test your new digital solution. This creates a controlled environment where you can collect real-world feedback, iron out the kinks, and measure the impact without disrupting your entire operation.
A successful pilot program does a few key things:
-
Validates the Solution: It proves the tech actually works as intended in your unique environment.
-
Builds Momentum: A “quick win” shows real value to stakeholders and gets more people excited and on board.
-
Provides Learning Opportunities: You’ll uncover unexpected challenges and user needs that will be invaluable for a wider rollout.
This infographic shows how these strategic moves translate directly into better business outcomes, cutting costs, boosting patient loyalty, and even opening up new revenue streams.
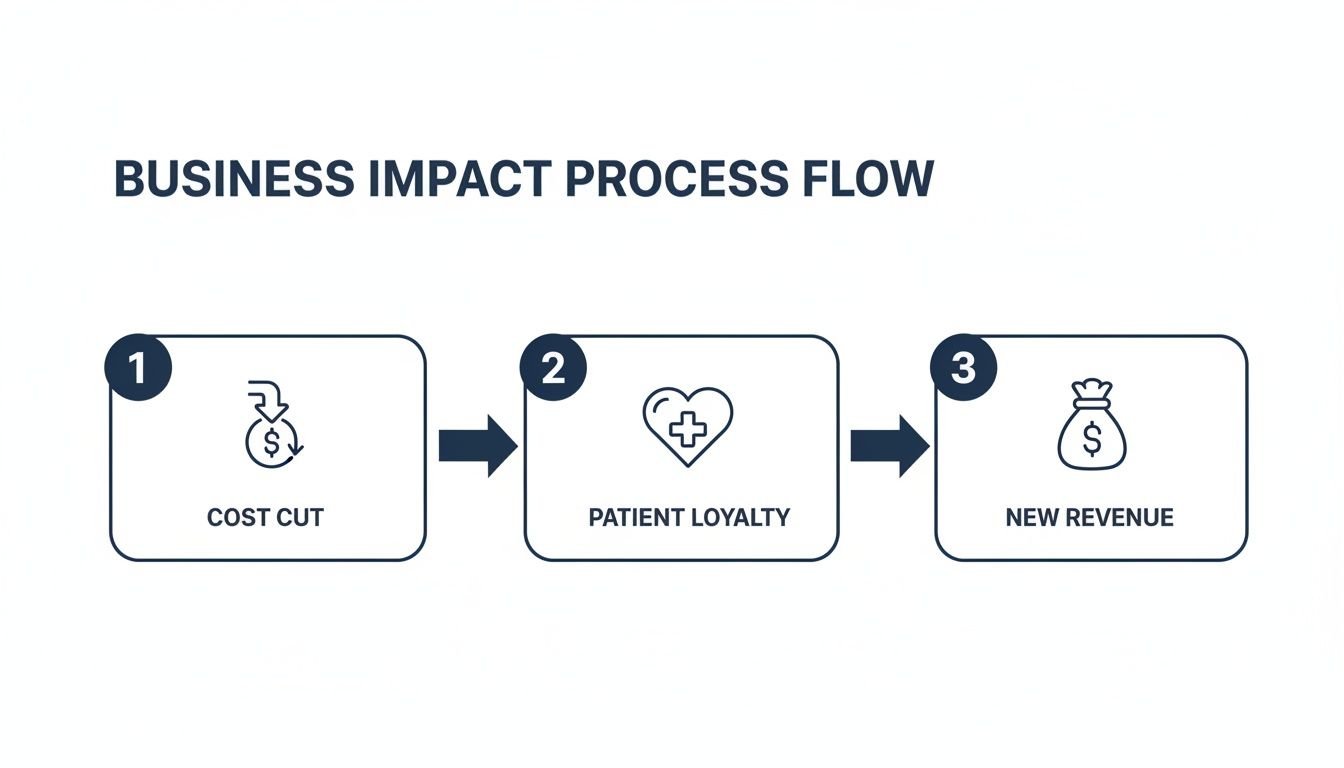
As this flow shows, digital initiatives aren’t just about the technology itself; they are direct drivers of your organization’s financial health and patient relationships.
Phase 4: Drive User Adoption and Continuous Improvement
The most brilliant technology in the world is completely useless if nobody uses it. This final phase is arguably the most important: making sure your team actually embraces the new tools. This takes way more than a one-off training session; it demands a real change management strategy.
Start by clearly communicating the “why” behind the shift. Show your staff how the new system will make their jobs easier, not just add another task to their plate. Get clinical champions involved – respected doctors and nurses who can advocate for the new technology with their peers. And finally, create clear channels for feedback and offer ongoing support.
Remember, transformation isn’t a project with an end date. It’s a continuous cycle of implementing, measuring, and refining. Use the data and feedback you gather to constantly improve your systems and processes. That’s how you stay agile and ready for whatever comes next.
See Digital Transformation in the Real World
It’s one thing to talk about strategies and roadmaps, but the real magic of healthcare digital transformation happens when you see it in action. This is where the theory meets reality, and we can witness how technology is truly changing lives – for both patients and providers. These stories are the tangible proof of what’s possible when a clear vision is paired with the right digital tools.
Let’s look at a couple of powerful examples that show how digital solutions are solving some of healthcare’s toughest challenges, delivering results you can measure. These are the kinds of successful outcomes we work to create in our own client cases.

Predictive Analytics Slashes Hospital Readmissions
Unplanned hospital readmissions are a stubborn and expensive problem. One major hospital system was watching too many patients return within 30 days of being sent home, especially those with chronic conditions like congestive heart failure. This put a huge strain on their resources and, more importantly, meant that post-discharge care wasn’t working as it should.
Their solution? A predictive analytics platform driven by machine learning. The system dug into decades of electronic health record (EHR) data to find subtle patterns and risk factors that even the most experienced clinician might overlook.
Here’s a breakdown of how it worked:
-
Data Integration: The platform gathered all sorts of information: patient demographics, lab results, medical history, and even social determinants of health, to get a complete picture.
-
Risk Scoring: As soon as a patient was admitted, the AI model calculated a “readmission risk score” in real-time, instantly flagging high-risk individuals for the care team.
-
Proactive Intervention: With this heads-up, care coordinators could step in before the patient was discharged. They provided personalized education, scheduled follow-up appointments, and arranged home health visits to ensure a smooth transition.
The results were stunning. Within the first year, the hospital cut its 30-day readmission rate by 25% for that high-risk group. This wasn’t just a win for patient health; it also led to massive cost savings, proving the direct ROI of smart healthcare software development.
Telehealth Expands Specialty Care to Rural Communities
For too long, your zip code has determined your access to quality healthcare. A regional health system serving a massive, sparsely populated area knew this problem all too well. Patients were driving hundreds of miles to see specialists like neurologists or cardiologists, which often meant diagnoses were delayed, and chronic diseases were poorly managed.
To close this gap, the system rolled out a telehealth program that went far beyond simple video calls. It was a fully integrated digital care model, built with custom software development to make the experience seamless.
Digital transformation isn’t just about efficiency in urban centers; it’s a powerful tool for health equity, ensuring everyone has access to high-quality care, regardless of their zip code.
The program linked rural primary care clinics directly with specialists at the main urban hospital. A local doctor could launch a virtual consultation, letting the specialist examine the patient, review diagnostic scans in real-time, and build a treatment plan together.
The impact was immediate and profound. The system reported a 40% jump in specialty care access for rural patients, who also saved a huge amount of time and money on travel. By bringing the expertise to the community, the health system completely changed the game for care quality and patient satisfaction. It’s a perfect illustration of how a smart approach to AI for your business can solve deep-seated operational and social issues.
These stories show that healthcare digital transformation is more than just a buzzword. It’s about using technology to solve real problems, create smarter ways of working, and build a healthcare system that is more effective and accessible for everyone. As an experienced AI solutions partner, we help organizations just like these turn these possibilities into reality.
Navigating the Challenges of Going Digital
Making the leap to a fully digital healthcare environment can bring incredible benefits, but let’s be honest, it’s not a simple flip of a switch. This journey is filled with potential hurdles, but knowing what they are ahead of time is the best way to turn those obstacles into strategic wins. The challenges aren’t just about technology; they’re deeply tied to people, security, and money. Tackling them head-on is how you build a new digital foundation that’s strong enough to last.
Fortifying Data Security and Ensuring Compliance
In healthcare, data isn’t just data. It’s a person’s most private information, and protecting it is everything. As organizations go digital, they naturally open up new doors for security risks. Every piece of patient information, from electronic health records to a simple telehealth call, has to be locked down tight against potential breaches.
Simply meeting regulations like HIPAA is the bare minimum, not the final goal. Real security goes beyond just having the right software; it demands a security-first culture. As we covered in our guide on HIPAA-compliant software development, this means ongoing training for every staff member, regular security audits, and solid encryption for all data, whether it’s sitting on a server or moving across the network. It also means adopting proven network security best practices to stay ahead of cyber threats that are always getting smarter.
A successful digital transformation treats cybersecurity as a core business function. It’s an ongoing commitment to protecting patient trust, not a one-time technical fix.
Overcoming Staff Resistance and Driving Adoption
Often, the toughest barrier isn’t the technology itself; it’s getting people to embrace it. Doctors, nurses, and administrative staff have their established routines, and any major change is bound to be met with some resistance. They might worry about their jobs, feel intimidated by the learning curve, or fear that technology will get in the way of their connection with patients. These are all completely valid concerns.
The key to getting everyone on board is smart change management. It really boils down to three things:
-
Communicate the ‘Why’: Don’t just show them a new tool; explain exactly how it will make their jobs easier, reduce paperwork, and ultimately help them provide better care.
-
Involve Clinical Champions: Find respected doctors or nurses who are excited about the change and empower them to lead the way and advocate for the new systems.
-
Provide Comprehensive Training: Offer plenty of hands-on training and make sure support is always available. When people feel confident using a tool, they’re far more likely to adopt it.
Managing Investment Costs and Proving ROI
The price tag for a full digital overhaul can be intimidating, particularly for smaller clinics or hospitals. The costs of new hardware, software licenses, and implementation support add up quickly, and getting budget approval can be tough without a clear financial plan.
A phased rollout is almost always the best way to go. Instead of trying to do everything at once, pick one area where you can make a big impact and start there. A pilot program makes the initial investment much more manageable and helps you prove a clear return on investment (ROI) much faster. For instance, launching an automated appointment scheduling system can immediately cut down on administrative hours, showing real savings. That success builds momentum and makes a powerful case for the next phase of your digital journey.
Answering Your Key Questions on Digital Health Transformation
As we wrap up, it’s natural to have a few lingering questions. Let’s tackle some of the most common ones we hear from healthcare leaders who are just starting to think about this kind of change.
Where On Earth Do We Even Begin?
The best place to start is right where you are. Take a hard look at your current operations and pinpoint the biggest headaches for your patients and your team. Is it the endless back-and-forth of scheduling? Or maybe the struggle to get the right clinical data in front of the right person at the right time?
Don’t try to boil the ocean. Pick one high-impact problem to solve first. A quick win builds momentum, proves the value of the investment, and gets everyone excited for what’s next.
How Can We Go Digital Without Compromising Patient Data Security?
This is non-negotiable, and security can’t be a feature you bolt on at the end. It has to be baked in from the very beginning. That means working exclusively with vendors who live and breathe HIPAA compliance, enforcing multi-factor authentication everywhere, and encrypting all patient data, whether it’s sitting on a server or moving across the network.
As we covered in our deep dive on building HIPAA-compliant software, technology is only half the battle. Regular security audits and ongoing staff training are absolutely essential to guard against simple human error.
Security in digital health is a continuous commitment to protecting patient trust. It’s an ongoing process of vigilance, not a one-time technical fix.
Is This Only for Big Hospitals With Huge Budgets?
Absolutely not. You don’t need a massive capital investment to get started. Many of the best tools are cloud-based platforms that operate on a subscription model (SaaS), which turns a huge upfront cost into a predictable operating expense.
For smaller practices, the key is to focus on solutions with a quick and clear return on investment. Think about telehealth platforms that expand your reach or automated tools that free up administrative staff. These often pay for themselves surprisingly fast through sheer efficiency gains.
Ready to modernize your healthcare operations? Bridge Global is your expert AI solutions partner, specializing in secure and compliant digital transformation. Let’s build the future of healthcare together.



